What Kind of Professionals Should I Be Seeing? 9 People You’ll Likely Work With in Mental Health and Addiction Recovery





Table of Contents
- 1. Therapists and counselors
- 2. Psychologists
- 3. Social workers
- 4. Medical providers
- 5. Peer recovery specialists
- 6. Holistic practitioners
- 7. Psychiatrists
- 8. Psychiatric nurse practitioners
- 9. Primary care providers (PCPs)
- Understanding credentials
- Telehealth vs. in-person options
- Find a treatment program
- FAQs
Recovering from an addiction or mental health condition is a team effort involving clinical, therapeutic, and medical professionals. But how do you know whom to add to the team? Where should you start?
We’ll explore who’s usually involved in mental health and addiction treatment, why they’re there, and how to find professionals who fit your recovery needs.
Understanding the Mental Health and Addiction Care Team
When you enter a mental health or addiction treatment program, you’ll likely work with several different professionals as part of your care team. The range can be broad, from psychiatrists and therapists to specialists in areas like trauma-informed yoga. While every program is different, there are a few core healthcare professionals you’re most likely to encounter.
Here’s who they are and why they’re considered essential to your recovery:
1. Therapists and Counselors
A therapist is a licensed mental health professional, typically with a master’s degree in counseling, social work, or marriage and family therapy (e.g., LPC, LCSW, LMFT). Therapists provide individual, couples, family, or group therapy, and many have additional training in specific modalities like Eye Movement Desensitization and Reprocessing (EMDR), cognitive behavioral therapy (CBT), or trauma-informed care. They support clients through various emotional and behavioral challenges, helping them build coping strategies, improve relationships, and enhance overall well-being.
Therapists are trained to address issues such as grief, life transitions, substance use, trauma, and more, always emphasizing safety, healing, and client empowerment.
Explore Alcohol Treatment Centers
2. Psychologists
A psychologist is a mental health professional1 with advanced training in human behavior, emotional processes, and mental disorders. Clinical psychologists hold a doctoral degree (Ph.D., Psy.D., or Ed.D.) and are licensed to assess, diagnose, and treat a wide range of psychological issues, including depression, anxiety, eating disorders, personality disorders, psychotic disorders, and more. They often provide evidence-based therapies and may also conduct psychological testing.
Psychologists work in diverse settings such as hospitals, clinics, rehabilitation centers, schools, and private practices.
3. Social Workers
Licensed clinical social workers (LCSWs)2 are trained mental health professionals who support patients both clinically and practically. In addition to providing therapy for substance use and mental health issues, they help patients manage the real-world logistics of recovery, like securing housing, applying for benefits, or coordinating follow-up care.
For example, if someone is transitioning out of inpatient treatment, an LCSW might help them find outpatient services, connect with support groups, or access community resources that ease the shift back into daily life. Their role is especially valuable for patients navigating complex systems or multiple levels of care.
4. Medical Providers
Medical providers attend to medical recovery needs, like managing withdrawals, side effects of substance use or medications, and ensuring any co-occurring conditions like diabetes stay treated while you’re recovering. Medical providers include doctors, nurses, psychiatric nurse practitioners, and other medical staff. Doctors and physicians can diagnose mental health disorders and provide some mental health services, including brief interventions, but typically, they’ll refer you to specialists or another level of care.
Their referral can often get you in quicker and help ensure treatment is covered by health insurance. Some health care providers, clinics, and rehabs may require a referral to begin treatment—check with admissions staff if this is necessary.
5. Peer Recovery Specialists
Peer recovery specialists, also known as peer support specialists or recovery coaches, use their own lived experiences with addiction and recovery to support others in their healing journey. These certified professionals provide mentorship, advocacy, and emotional support. They can help patients feel understood, reduce feelings of isolation, and model the possibility of long-term recovery.
While support workers don’t provide clinical care, their guidance is rooted in shared experience and often complements therapy or medical treatment. Peer support improves engagement in treatment3 and increases the likelihood of sustained recovery.
6. Holistic Practitioners
Holistic practitioners focus on treating the whole person—mind, body, and spirit. In a treatment setting, this might include yoga instructors, mindfulness teachers, massage therapists, Reiki practitioners, or nutritionists. These providers use evidence-informed and complementary therapies to promote emotional regulation, physical healing, and stress relief.
Holistic care isn’t a substitute for clinical treatment, but it can help patients reconnect with their bodies, build healthy routines, and find meaning in the recovery process.
Who Can Prescribe Medication?
A prescriber is different from a therapist. While your prescriber will prescribe medications and work with you to ensure they’re effective, a therapist handles the emotional, processing, and goal-setting side of recovery. They cannot prescribe medications of any kind.
These professionals can prescribe medication:
7. Psychiatrists
Psychiatrists have a deep, comprehensive knowledge of the brain’s chemistry and neurological functioning, and what chemicals or processes need to be corrected for someone to feel better. They know which medications will work for specific conditions, adjusting the type or dose to fit your unique symptoms.
It can take a few sessions to get the dose and type of medication right, as most psych meds take 2+ weeks to take effect, but the results can be life-changing. Once you find the right medication(s) for you, sessions with your psychiatrist will look more like check-ins to see if you’ve had any change in tolerance, any side effects, or want to start tapering off the medication.
Note: Most psychologists are not licensed to prescribe medication because they are not medical doctors. However, in a few U.S. states, licensed psychologists can prescribe certain psychiatric medications after completing additional education and certification in clinical psychopharmacology. While these exceptions exist, prescribing medication remains primarily within the scope of psychiatrists, who are medical doctors and licensed to prescribe in all states.
8. Psychiatric Nurse Practitioners
All psychiatric nurse practitioners can prescribe medications,4 but in some states, they also need a collaborating physician to approve the order. Psychiatric nurse practitioners are not doctors, but they do have advanced training in mental health and psychiatry. When looking for this type of support, oftentimes a referral from your PCP can be a great place to start.
9. Primary Care Providers (PCPs)
Your PCP, or primary care physician, is who you go to when you’re sick or something isn’t feeling right. Every PCP’s comfort level with psychiatric medications varies. Some don’t feel comfortable prescribing medications beyond SSRIs or SNRIs. In these cases, they’ll refer you to psychiatry for mood stabilizers, antipsychotics, sleep medications, or stimulants. Experts recommend that people taking mental health and psychiatric medications get medication management support from psychiatrists, psychiatric nurse practitioners, or specialized treatment providers.
Learn more about medication management and why it’s important to the recovery process.
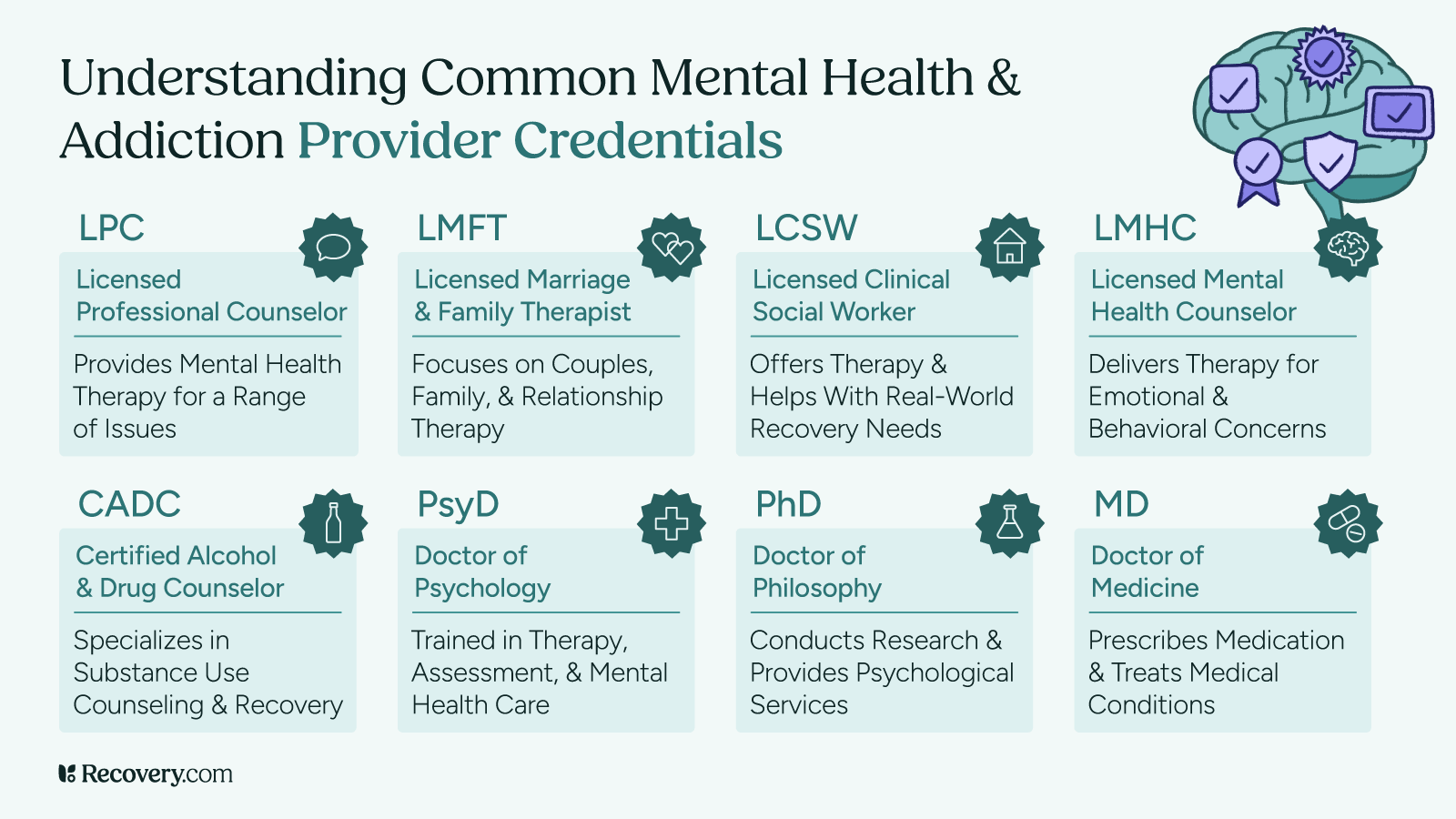
Credentials to Look For
Almost everyone on your treatment team should have credentials of some sort. If they don’t, that’s a red flag. Here are the types of credentials and licensure reputable providers will have:
- LCSW: Licensed clinical social worker; specializes in mental health support and case management
- LMFT: Licensed marriage and family therapist; trained to work with couples, families, and relationship dynamics
- CADC: Certified addiction counselor; specializes in addiction and substance use treatment
- LMHC: Licensed mental health counselor; offers therapy for a wide range of mental health conditions.
- LPC: Licensed professional counselor; similar to LMHC, depending on the state
- Ph.D: Doctor of Philosophy; often held by psychologists who provide therapy or conduct psychological testing and research
- M.D: Doctor of Medicine; held by psychiatrists and physicians who can prescribe medication
- State medical license, Psy.D., and board certification: Required for psychiatrists and physicians to practice and prescribe legally
When You Need a Team, Not Just One Person
Coordinated care is a quiet hero in addiction and mental health treatment. This means everyone in your treatment team is working towards a goal together, not siloed. Coordinated care ensures that each area of your recovery moves towards that goal and doesn’t accidentally minimize or negatively interact with another.
Having a team is especially vital for patients with co-occurring disorders: a mental health condition and a substance use disorder, 2 different mental health conditions, 2 different substance use disorders, or any other combination of conditions.
The nature of mental illness and substance use increases the demand for a coordinated treatment plan. Each person experiences their diagnosis differently and resonates with treatment in their own ways. Multiple, coordinated interventions, like therapy, medication, peer support, life skills education, and family therapy, can be even more effective.
Going to a residential treatment center or outpatient clinic means you benefit from coordinated care, with your treatment team meeting regularly to discuss your case. Not every treatment provider focuses strongly on coordination, but many do.
Telehealth vs. In-Person Options
Telehealth has broadened the reach of behavioral health care, allowing more people than ever before to get treatment. Telehealth is especially vital for rural populations5 and people with mobility challenges. In-person care, however, has many benefits—mainly the face-to-face human connection it provides.
Telehealth Pros and Cons
A major pro for telehealth is its flexibility. You don’t need to drive anywhere, worry about parking, or live anywhere close to a physical treatment center. You only need a device (like a phone or laptop) and an internet connection. Telehealth is usually covered by insurance, same as in-person. You can connect with experts worldwide, broadening your access to treatment.
A con is that it can be harder to form a connection with someone virtually, which is a vital component of the therapeutic alliance. Some say it’s harder to communicate or feel seen in a virtual setting, leading to poorer treatment outcomes.6 Internet issues and technical problems can also disrupt sessions.
In-Person Pros and Cons
A pro for in-person care is the ability to communicate and connect more comprehensively. This means nonverbal communication and body language, which your therapist can use to make your sessions more effective. For example, if you’re wringing your hands and fidgeting, they’ll know to switch topics or gently explore what’s making you uncomfortable.
Time commitment is a con for in-person care. In addition to the session itself, you have to get ready, drive there, park, and drive home. The total time commitment can be twice as long as the appointment itself, even longer for those in rural areas. In-person treatment options can also be limited since centers and clinics must be physically close to you.
Both telehealth and in-person care can help you heal. The best setting for you will depend on your preferences, location, and insurance coverage.
“The choice is yours.”
Recovery isn’t always easy, but the rewards are well worth it. Kai, whose recovery led him out of addiction and homelessness and into a life of stability and purpose, has this question for people considering a change:
How free do you want to be? Do you want to just be sober, or do you want to be fulfilled and sober? The choice is yours. It takes a little bit of work, but it never killed anybody. And I guarantee yo, you’ll be pleased with what you got. You might even get more than you bargain for.
Teaming Up for Recovery
Recovery isn’t a one-person show. And that’s a good thing.
You aren’t meant to do it alone. Imagine each team member—a therapist, doctor, psychiatrist—extending a hand in support. The more hands, the stronger your treatment, and the less you have to carry alone.
Start today: Use Recovery.com to find the best treatment for you and your needs.
FAQs
Q: What professionals deal with mental health?
A: Types of mental health professionals include psychologists, psychiatrists, licensed professional counselors (LPCs), clinical social workers, marriage and family therapists, and psychiatric nurse practitioners. Each has different training and specialties.
Q: Is it better to see a psychologist or psychiatrist?
A: It depends on your needs. Psychiatrists can prescribe medication and are often ideal for complex or severe mental illnesses. Psychologists focus more on talk therapy, testing, and long-term emotional support.
Q: Which type of professional works with individuals with severe mental disorders?
A: Psychiatrists and clinical psychologists often specialize in treating severe mental illnesses such as schizophrenia, bipolar disorder, and major depression. These professionals may work in inpatient or outpatient settings.
Q: Should I see an LPC or psychologist?
A: LPCs are trained in counseling strategies and are excellent for talk therapy and everyday mental health challenges. Psychologists may be more suitable for psychological testing, trauma recovery, or complex mental health diagnoses.
Q: How do I choose a mental health professional?
A: Consider your goals (e.g., therapy, medication, diagnosis), the provider’s credentials, experience, and whether they specialize in your area of concern. Look for licensed providers and check reviews or referrals.
Q: What is substance abuse counseling?
A: Substance abuse counseling focuses on helping individuals overcome addiction and build healthier lifestyles. It often includes therapy, relapse prevention, and support for co-occurring disorders like depression or anxiety.
Q: What is psychiatry?
A: Psychiatry is a medical field that deals with diagnosing, treating, and preventing mental illnesses. Psychiatrists are medical doctors who can prescribe medications and may provide psychotherapy.
Q: What types of addiction specialists are available for treatment?
A: Addiction specialists include substance abuse counselors, addiction medicine doctors, psychiatrists with addiction training, certified peer recovery specialists, and licensed therapists with substance use expertise.
Q: What kind of therapist should I see for addiction recovery?
A: Look for a licensed professional counselor, social worker, or psychologist who specializes in addiction, dual diagnosis, or trauma-informed care. Many use evidence-based therapies like CBT or motivational interviewing.
Q: What professionals can help with both mental health and addiction issues?
A: Addiction psychiatrists and licensed therapists trained in co-occurring disorders can address both areas. Integrated treatment programs also offer coordinated care from multiple professionals.
-
"psychologist." APA Dictionary of Psychology. https://dictionary.apa.org/.
-
Clinical Social Work. https://www.socialworkers.org/Practice/Clinical-Social-Work. Accessed 26 June 2025.
-
Jones, Nev, et al. “Peer Support, Self-Determination, and Treatment Engagement: A Qualitative Investigation.” Psychiatric Rehabilitation Journal, vol. 36, no. 3, 2013, pp. 209–14. APA PsycNet, https://doi.org/10.1037/prj0000008.
-
American Medical Association. (2023). State law chart: Nurse practitioner prescriptive authority. https://www.ama-assn.org/sites/ama-assn.org/files/corp/media-browser/specialty%20group/arc/ama-chart-np-prescriptive-authority.pdf
-
Butzner, Michael, and Yendelela Cuffee. “Telehealth Interventions and Outcomes Across Rural Communities in the United States: Narrative Review.” Journal of Medical Internet Research, vol. 23, no. 8, Aug. 2021, p. e29575. www.jmir.org, https://doi.org/10.2196/29575.
-
Moudatsou M, Stavropoulou A, Rovithis M, Koukouli S. Evaluation of Online Counseling through the Working Experiences of Mental Health Therapists Amidst the COVID-19 Pandemic. Healthcare (Basel). 2024 Feb 19;12(4):495. doi: 10.3390/healthcare12040495. PMID: 38391870; PMCID: PMC10888081.
Our Promise
How Is Recovery.com Different?
We believe everyone deserves access to accurate, unbiased information about mental health and recovery. That’s why we have a comprehensive set of treatment providers and don't charge for inclusion. Any center that meets our criteria can list for free. We do not and have never accepted fees for referring someone to a particular center. Providers who advertise with us must be verified by our Research Team and we clearly mark their status as advertisers.
Our goal is to help you choose the best path for your recovery. That begins with information you can trust.







