What Kind of Professionals Should I Be Seeing? 9 People You’ll Likely Work With in Mental Health and Addiction Recovery



As a Clinical Research Specialist, writer, and person with lived experience in mental health recovery, Grace blends clinical research with honest storytelling to inspire healing and hope. In her free time, she enjoys writing books for young adults, an age when she needed stories the most.

Dr. Mala, is the Chief Clinical Officer at Recovery.com, where she develops impartial and informative resources for people seeking addiction and mental health treatment.




As a Clinical Research Specialist, writer, and person with lived experience in mental health recovery, Grace blends clinical research with honest storytelling to inspire healing and hope. In her free time, she enjoys writing books for young adults, an age when she needed stories the most.

Dr. Mala, is the Chief Clinical Officer at Recovery.com, where she develops impartial and informative resources for people seeking addiction and mental health treatment.
Table of Contents
- Understanding the Mental Health and Addiction Care Team
- 1. Therapists
- 2. Psychologists
- 3. Social Workers
- 4. Medical Providers
- 5. Peer Recovery Specialists
- 6. Holistic Practitioners
- Who Can Prescribe Medication?
- 7. Psychiatrists
- 8. Psychiatric Nurse Practitioners
- 9. Primary Care Providers (PCPs)
- Credentials to Look For
- When You Need a Team, Not Just One Person
- Telehealth vs. In-Person Options
- Teaming Up for Recovery
Recovering from a substance use disorder or a mental health condition, it is important to have a diverse team of qualified, dedicated professionals there to support you. But, it can be difficult to identify who should be involved in your treatment, especially if you are getting care for the first time.
Here, we’ll explore which professionals are usually involved in mental health and addiction treatment, why they’re there, and how you can find professionals who fit your recovery needs.
Understanding the Mental Health and Addiction Care Team
When you enter into a mental health or addiction treatment program, you’ll be receiving care from a variety of professionals in the field. These professionals can range from psychiatrists and therapists to specialists in niche areas like trauma-informed yoga. While every program is different, there are a few core healthcare professionals you’ll most likely encounter.
Here’s who they are and why they’re considered essential to your recovery:
1. Therapists
Therapists are people who have received training in and who practice a variety of therapies designed to help treat mental or physical disorders or diseases. These are licensed mental health professionals who hold a master’s degree in a relevant field, such as social work or marriage and family therapy.1
Therapists provide individual, couples, family, or group therapies, and many have additional training in specific modalities like eye movement desensitization and reprocessing (EMDR), cognitive behavioral therapy (CBT), or trauma-informed care. They support clients through various emotional and behavioral challenges, helping them build coping strategies, improve relationships, and enhance overall well-being.
Therapists are trained to address issues such as grief, life transitions, substance use, trauma, and more, always emphasizing safety, healing, and client empowerment.
2. Psychologists
A psychologist is a mental health professional with advanced training in human behavior, emotional processes, and mental disorders.2 Psychologists hold a doctoral degree (Ph.D., Psy.D., or Ed.D.) and are licensed to assess, diagnose, and treat a wide range of psychological issues, including depression, anxiety, eating disorders, personality disorders, psychotic disorders, and more. They often provide evidence-based therapies and may also conduct psychological testing.
Psychologists work in diverse settings such as hospitals, clinics, rehabilitation centers, schools, and private practices.

3. Social Workers
Licensed clinical social workers (LCSWs) are trained mental health professionals who support patients both clinically and practically.3 In addition to providing therapy for substance use and mental health issues, they help patients manage the real-world logistics of recovery, like securing housing, applying for benefits, or coordinating follow-up care.
For example, if someone is transitioning out of inpatient treatment, an LCSW might help them find outpatient services, connect with support groups, or access community resources that ease the shift back into daily life. Their role is especially valuable for patients navigating complex systems or multiple levels of care.
4. Medical Providers
Medical providers attend to medical recovery needs, like managing the detox process, treating side effects of substance use, or providing medications while ensuring any co-occurring physical health conditions (e.g., diabetes, high cholesterol) are simultaneously treated during your recovery. Medical providers include doctors, nurses, psychiatric nurse practitioners, and other medical staff. Doctors and physicians can diagnose mental health disorders and provide some mental health services, including brief interventions, but typically, they’ll refer you to specialists or another level of care.
Their referral can often get you in quicker and help ensure treatment is covered by health insurance. Some health care providers, clinics, and rehabs may require a referral to begin treatment—check with admissions staff if this is necessary.
5. Peer Recovery Specialists
Peer recovery specialists, also known as peer support specialists or recovery coaches, use their own lived experiences with addiction and recovery to support others in their healing journey. These certified professionals provide mentorship, advocacy, and emotional support. They can help patients feel understood, reduce feelings of isolation, and model the possibility of long-term recovery.
While peer recovery specialists don’t provide clinical care, their guidance is rooted in shared experience and often complements therapy or medical treatment. Peer support has been shown to improve engagement in treatment and increases the likelihood of sustained recovery.4
6. Holistic Practitioners
Holistic practitioners focus on treating the whole person—mind, body, and spirit. In an addiction or mental health treatment setting, this might include yoga instructors, mindfulness teachers, massage therapists, Reiki practitioners, or nutritionists. These providers use evidence-informed and complementary therapies to promote emotional regulation, physical healing, and stress relief.
Holistic care isn’t a substitute for clinical treatment, but it can help patients reconnect with their bodies, build healthy routines, and find meaning in the recovery process.
Who Can Prescribe Medication?
While a therapist handles the emotional, processing, and goal-setting side of recovery, a clinical professional who can prescribe medication can help treat the biological components of your recovery if necessary.
7. Psychiatrists
Psychiatrists have a deep, comprehensive knowledge of the brain’s chemistry and neurological functioning, as well as what chemicals or processes need to be corrected for someone to feel better. They know which medications will work for specific conditions, and are skilled in adjusting the type or dose to fit your unique symptoms.
Depending on the medication, it might take a few sessions to get the dose and type of medication right, as some psychiatric medications can take time to take full effect. Once you find the right medication(s) for you, sessions with your psychiatrist will look more like check-ins to see if you’ve had any change in tolerance, any side effects, or want to start tapering off the medication.
Note: Most psychologists are not licensed to prescribe medication because they are not medical doctors. However, in a few U.S. states, licensed psychologists can prescribe certain psychiatric medications after completing additional education and certification in clinical psychopharmacology. While these exceptions exist, prescribing medication remains primarily within the scope of psychiatrists, who are medical doctors and licensed to prescribe in all states.
8. Psychiatric Nurse Practitioners
All psychiatric nurse practitioners can prescribe medications, but in some states, they also need a collaborating physician to approve the order.5 Psychiatric nurse practitioners are not doctors, but they do have advanced training in mental health and psychiatry. When looking for this type of support, oftentimes a referral from your primary care physician can be a great place to start.
9. Primary Care Providers (PCPs)
Your PCP, or primary care physician, is who you go to when you’re sick or something isn’t feeling right. Every PCP’s comfort level with psychiatric medications varies. Some don’t feel comfortable prescribing medications beyond SSRIs or SNRIs. In these cases, they’ll provide you with a psychiatric treatment referral, where a professional can help you develop a plan for medications, such as mood stabilizers, antipsychotics, sleep medications, or stimulants (depending on your needs). Experts recommend that people taking mental health and psychiatric medications get medication management support from psychiatrists, psychiatric nurse practitioners, or specialized treatment providers.
Learn more about medication management and why it’s important to the recovery process.
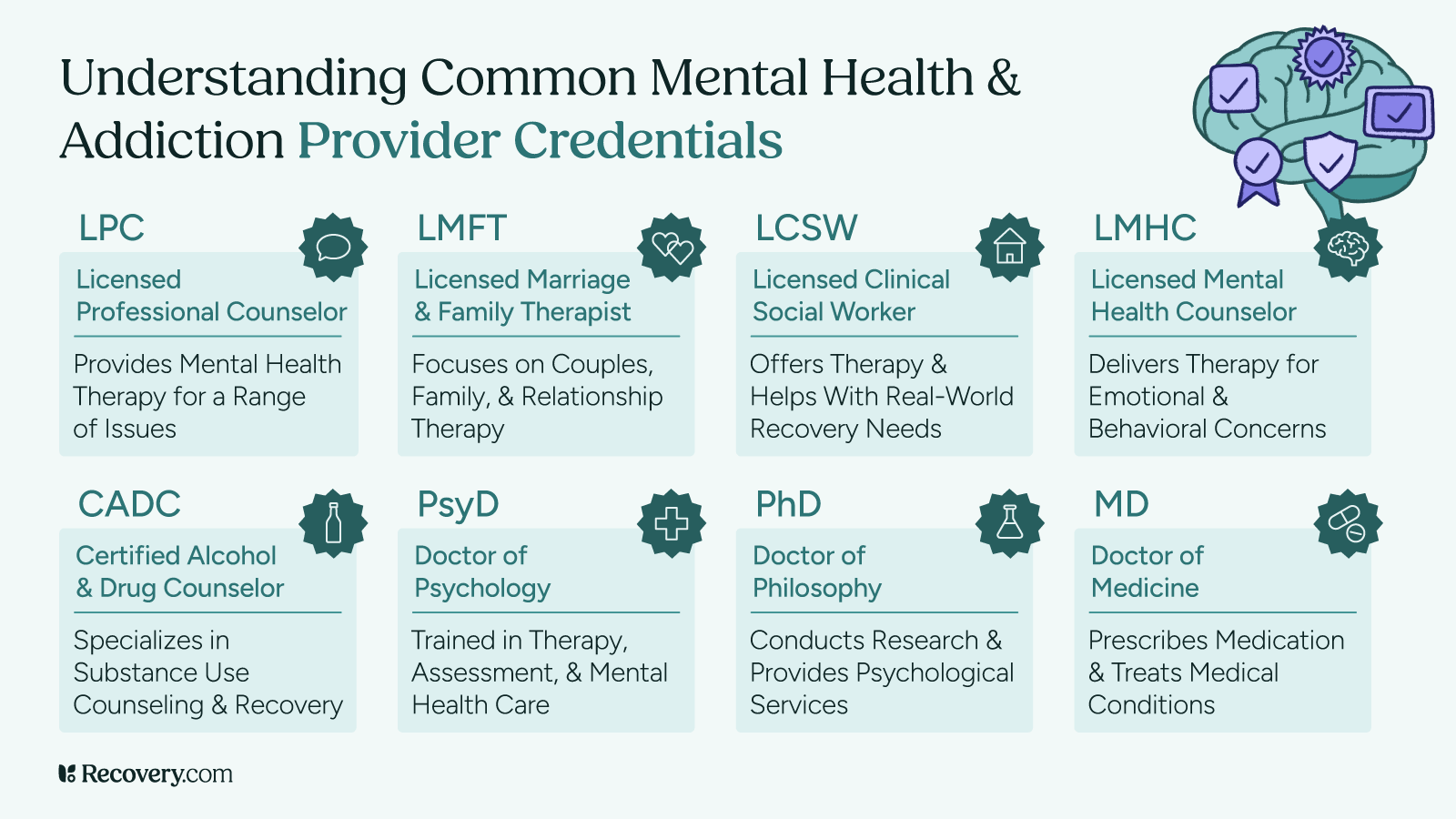
Credentials to Look For
Almost everyone on your treatment team should have credentials of some sort. If you are receiving treatment and find that many providers do not have the appropriate credentials, it is important to take a step back and reevaluate the care you are receiving.
Here are some of the types of credentials and licensures reputable providers will have:
- LCSW: Licensed clinical social worker; specializes in mental health support and case management
- LMFT: Licensed marriage and family therapist; trained to work with couples, families, and relationship dynamics
- CADC: Certified addiction counselor; specializes in addiction and substance use treatment
- LMHC: Licensed mental health counselor; offers therapy for a wide range of mental health conditions.
- LPC: Licensed professional counselor; similar to LMHC, depending on the state
- Ph.D: Doctor of Philosophy; often held by psychologists who provide therapy or conduct psychological testing and research
- M.D.: Doctor of Medicine; held by psychiatrists and physicians who can prescribe medication
- State medical license, Psy.D., and board certification: Required for psychiatrists and physicians to practice and prescribe legally
When You Need a Team, Not Just One Person
Coordinated care is a quiet hero in addiction and mental health treatment. This means everyone in your treatment team is working cohesively on your care. Coordinated care ensures that each area of your recovery moves towards your goals and doesn’t accidentally minimize or negatively interact with another.
Having a team is especially vital for patients with co-occurring disorders, which is defined as a mental health condition and a substance use disorder occurring at the same time.
The nature of mental illness and substance use increases the demand for a coordinated treatment plan. Each person experiences their diagnosis differently and resonates with treatment in their own ways. Multiple, coordinated interventions, like therapy, medication, peer support, life skills education, and family therapy, can be even more effective.
Going to a residential treatment center or outpatient clinic means you benefit from coordinated care, with your treatment team meeting regularly to discuss your case. Not every treatment provider focuses strongly on coordination, but many do.
Telehealth vs. In-Person Options
Telehealth has broadened the reach of behavioral health care, allowing more people than ever before to get treatment. Telehealth is especially vital for rural populations and people with mobility challenges.6 In-person care, however, has many benefits—mainly the face-to-face human connection it provides.
Telehealth Pros and Cons
A major pro for telehealth is its flexibility. You don’t need to drive anywhere, worry about parking, or live anywhere close to a physical treatment center. You only need a device (like a phone or laptop) and an internet connection. Telehealth is usually viewed as the same as an in-person appointment, therefore usually covered by insurance. You can connect with experts worldwide, broadening your access to treatment.
That being said, many find it more difficult to form a connection with someone virtually, which is a vital component of the therapeutic alliance. Some say it’s harder to communicate or feel seen in a virtual setting, possibly leading to poorer treatment outcomes.7 Internet issues and technical problems can also disrupt sessions and become a barrier for treatment.
In-Person Pros and Cons
When participating in in-person care, you have the ability to communicate and connect more comprehensively. This include nonverbal communication and body language, which your therapist can use to make your sessions more effective. For example, if you’re wringing your hands and fidgeting, they’ll know to switch topics or gently explore what’s making you uncomfortable.
Time commitment can be a challenge for in-person care. In addition to the session itself, you have to get ready, drive there, park, and drive home. The total time commitment can be twice as long as the appointment itself, even longer for those in rural areas. In-person treatment options can also be limited since centers and clinics may not be nearby to your home.
All things considered, both telehealth and in-person care can help you heal. The best setting for you will depend on your preferences, location, and insurance coverage.
Teaming Up for Recovery
Recovery isn’t a one-person show. And that’s a good thing.
You aren’t meant to do it alone. Imagine each team member—a therapist, doctor, psychiatrist—extending a hand in support. The more hands, the stronger your treatment, and the less you have to carry alone.
Start today: Use Recovery.com to find the best treatment for you and your needs.
FAQs
-
"Therapist." APA Dictionary of Psychology. https://dictionary.apa.org/therapist
-
American Psychological Association. (2018) April 19 . Psychologist. APA Dictionary of Psychology. https://dictionary.apa.org/
-
National Association of Social Workers. (n.d.). Clinical Social Work. https://www.socialworkers.org/Practice/Clinical-Social-Work
-
Corrigan, P.W., James, D., Jones, N., Larson, N., Parker, J. (2013). Peer support, self-determination, and treatment engagement: A qualitative investigation. Psychiatric Rehabilitation Journal, 36(3), 209–214. https://psycnet.apa.org/doiLanding?doi=10.1037%2Fprj0000008
-
American Medical Association. (2017). State law chart: Nurse practitioner Prescriptive Authority. https://www.ama-assn.org/sites/ama-assn.org/files/corp/media-browser/specialty%20group/arc/ama-chart-np-prescriptive-authority.pdf
-
Butzner, M., Cuffee, Y. (2021) August 26. Telehealth Interventions and Outcomes Across Rural Communities in the United States: Narrative Review. https://pubmed.ncbi.nlm.nih.gov/34435965/
-
Koukouli, S., Moudatsou, M., Rovithis, M., Stavropoulou, A. (2024) February 9. Evaluation of Online Counseling through the Working Experiences of Mental Health Therapists Amidst the COVID-19 Pandemic. https://pubmed.ncbi.nlm.nih.gov/38391870/
Our Promise
How Is Recovery.com Different?
We believe everyone deserves access to accurate, unbiased information about mental health and recovery. That’s why we have a comprehensive set of treatment providers and don't charge for inclusion. Any center that meets our criteria can list for free. We do not and have never accepted fees for referring someone to a particular center. Providers who advertise with us must be verified by our Research Team and we clearly mark their status as advertisers.
Our goal is to help you choose the best path for your recovery. That begins with information you can trust.










