Sensory Overload ADHD: Understand Triggers and Learn Coping Strategies



Dr. Glowiak has a PhD in counselor education and supervision and has served those struggling with addiction while continuing to spread awareness on the topic to students, clinicians, instructors, and the general public.

Dr. Mala, is the Chief Clinical Officer at Recovery.com, where she develops impartial and informative resources for people seeking addiction and mental health treatment.




Dr. Glowiak has a PhD in counselor education and supervision and has served those struggling with addiction while continuing to spread awareness on the topic to students, clinicians, instructors, and the general public.

Dr. Mala, is the Chief Clinical Officer at Recovery.com, where she develops impartial and informative resources for people seeking addiction and mental health treatment.
Imagine walking into a bustling caf�the chatter of conversations, the clinking of dishes, and the aroma of freshly brewed coffee all collide in a sensory whirlwind. For individuals with ADHD, this scene can quickly escalate into an overwhelming experience known as sensory overload.
This phenomenon not only makes everyday environments feel chaotic but can also hinder focus and emotional well-being. As we delve into the intricate world of sensory overload in ADHD, we’ll explore how it affects people’s lives and uncover effective strategies to navigate this sensory storm.
What Is ADHD?
Attention Deficit Hyperactivity Disorder (ADHD) is a neurodevelopmental mental health disorder characterized by persistent patterns of inattention, hyperactivity, and impulsivity that interfere with functioning or development.
According to the DSM-5-TR (Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision), the traditional signs and symptoms of ADHD are categorized into two main groups: inattention and hyperactivity-impulsivity.1
Symptoms of inattention may include difficulty sustaining attention, frequent careless mistakes in schoolwork or other activities, difficulty organizing tasks, avoidance of tasks that require sustained mental effort, and forgetfulness in daily activities. Symptoms of hyperactivity-impulsivity may include fidgeting, difficulty remaining seated, excessive talking, interrupting others, and acting without thinking.
To receive a diagnosis, these symptoms must be present for a minimum of six months and must be evident in more than one setting, such as at home and school. Understanding ADHD is essential for providing effective support and interventions for those affected by it.
The ADHD Brain
The ADHD brain exhibits distinct neurobiological differences that influence attention, impulse control, and emotional regulation.2 Neuroimaging studies have shown that individuals with ADHD often demonstrate variations in brain structure and function compared to neurotypical individuals.
Key areas affected include the prefrontal cortex, which is responsible for executive functions such as decision-making and impulse control; the basal ganglia, which play a role in regulating movement and attention; and the cerebellum, which is involved in coordination and the processing of sensory information. Research shows that individuals with ADHD may have decreased dopamine levels in these regions, which can contribute to difficulties in motivation, focus, and reward processing.
Differences Depending on Age
In children, ADHD symptoms may present as hyperactivity and impulsivity, which are often more pronounced due to the ongoing neurodevelopmental processes in their brains.3 As children transition into adolescence, there may be a shift in symptoms, with increased challenges in attention and emotional regulation.
Neurological growth spurts during adolescence can lead to further changes in brain connectivity and working memory capabilities, marking a period where individuals with ADHD may face heightened emotional responses and social pressures.
In adults, the manifestation of ADHD often changes again, with hyperactive symptoms typically diminishing but challenges in attention, organization, and emotional self-regulation becoming more prominent.4
The adult ADHD brain may demonstrate adaptive behaviors developed over time, but individuals may still experience residual symptoms that impact daily functioning and quality of life.
How have you professionally supported someone with ADHD experiencing sensory overload, and what strategies proved most effective?

What Is Sensory Overload?
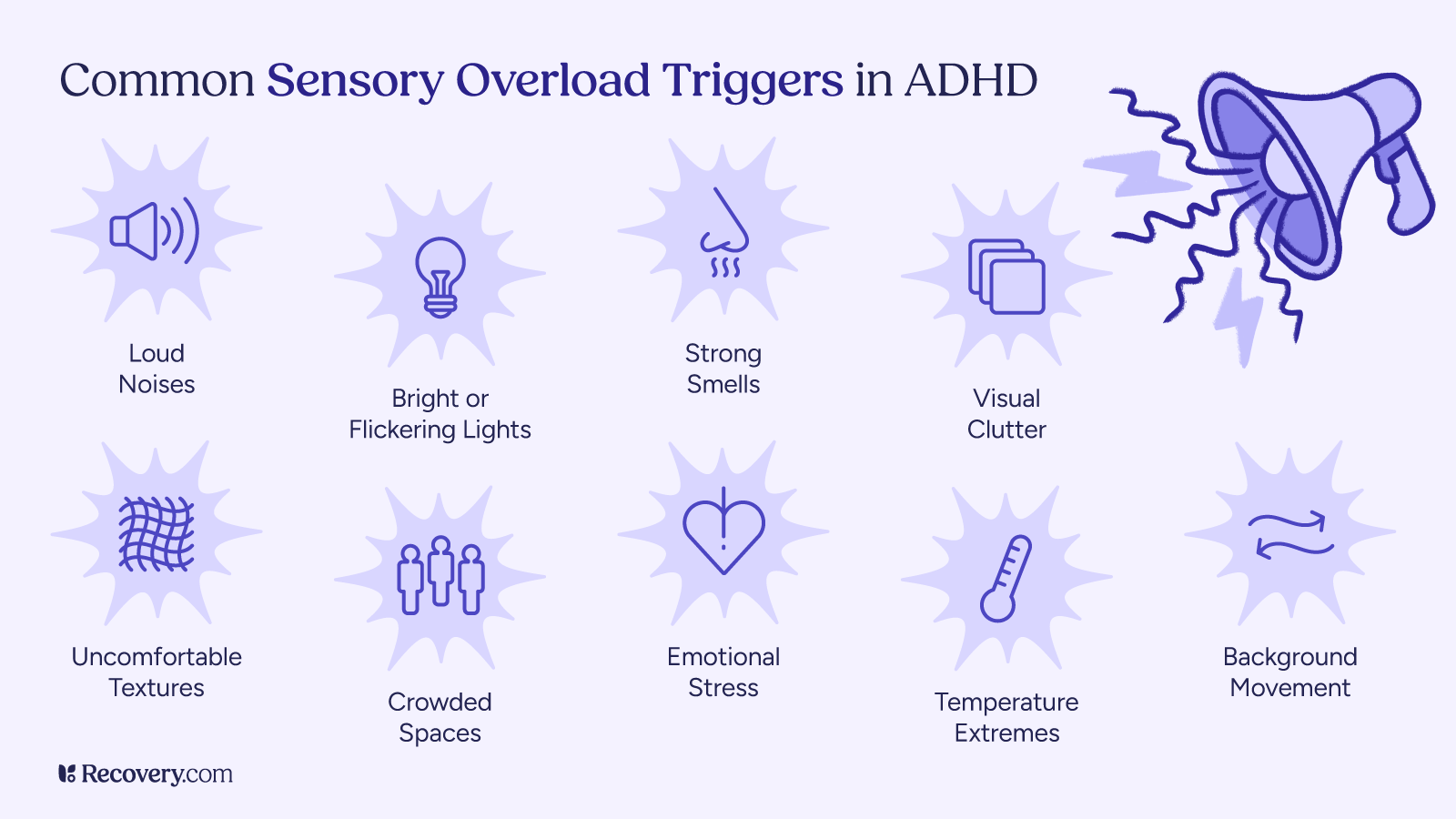
Sensory overload or overstimulation in the context of ADHD occurs when an individual experiences an overwhelming amount of sensory input—whether from sights, sounds, textures, or even strong smells like perfumes—making it difficult to concentrate or cope with the environment.5 For those with ADHD, heightened sensitivity to sensory stimuli can lead to feelings of anxiety, irritability, and fatigue.
Here’s a closer look at some common symptoms of sensory overload, along with relatable examples:
- Inability to Focus: Struggling to concentrate on a conversation at a party because of the loud music and chatter surrounding you.
- Feeling Overwhelmed: Walking into a busy shopping mall and feeling anxious or drained due to the bright lights and multiple noises happening at once.
- Irritability: Becoming easily frustrated or upset when trying to work in a noisy café, where the sounds make it hard to think.
- Physical Discomfort: Becoming irritated by the tags on your clothing or the texture of certain fabrics, leading you to rip off your shirt in discomfort.
- Panic or Anxiety Attacks: Experiencing a sudden rush of panic when in a crowded space, causing you to feel trapped and needing to escape.
- Processing Challenges: Having trouble following a lecture because your mind is racing from the sounds and movements around you.
- Avoidance Behavior: Choosing to stay at home instead of attending social events because you fear being overwhelmed by the environment.
Recognizing these symptoms can help individuals with ADHD, as well as their friends and family, develop effective coping strategies and create more supportive environments. Understanding sensory overload is key to managing it effectively and improving overall well-being.

Sensory Processing Disorder (SPD)
Sensory Processing Disorder (SPD) refers to a condition where the brain has difficulty receiving and responding to sensory information from the environment.6 Individuals with SPD may overreact, underreact, or have unusual responses to sensory stimuli, such as sounds, flashing lights, textures, or tastes. This is called sensory over-responsivity. This can lead to challenges in daily activities, social interactions, and emotional regulation.
SPD can occur independently or alongside other conditions, such as ADHD or autism spectrum disorder (ASD). Treatment often involves occupational therapy, which focuses on improving sensory integration and coping strategies to enhance daily functioning and quality of life.
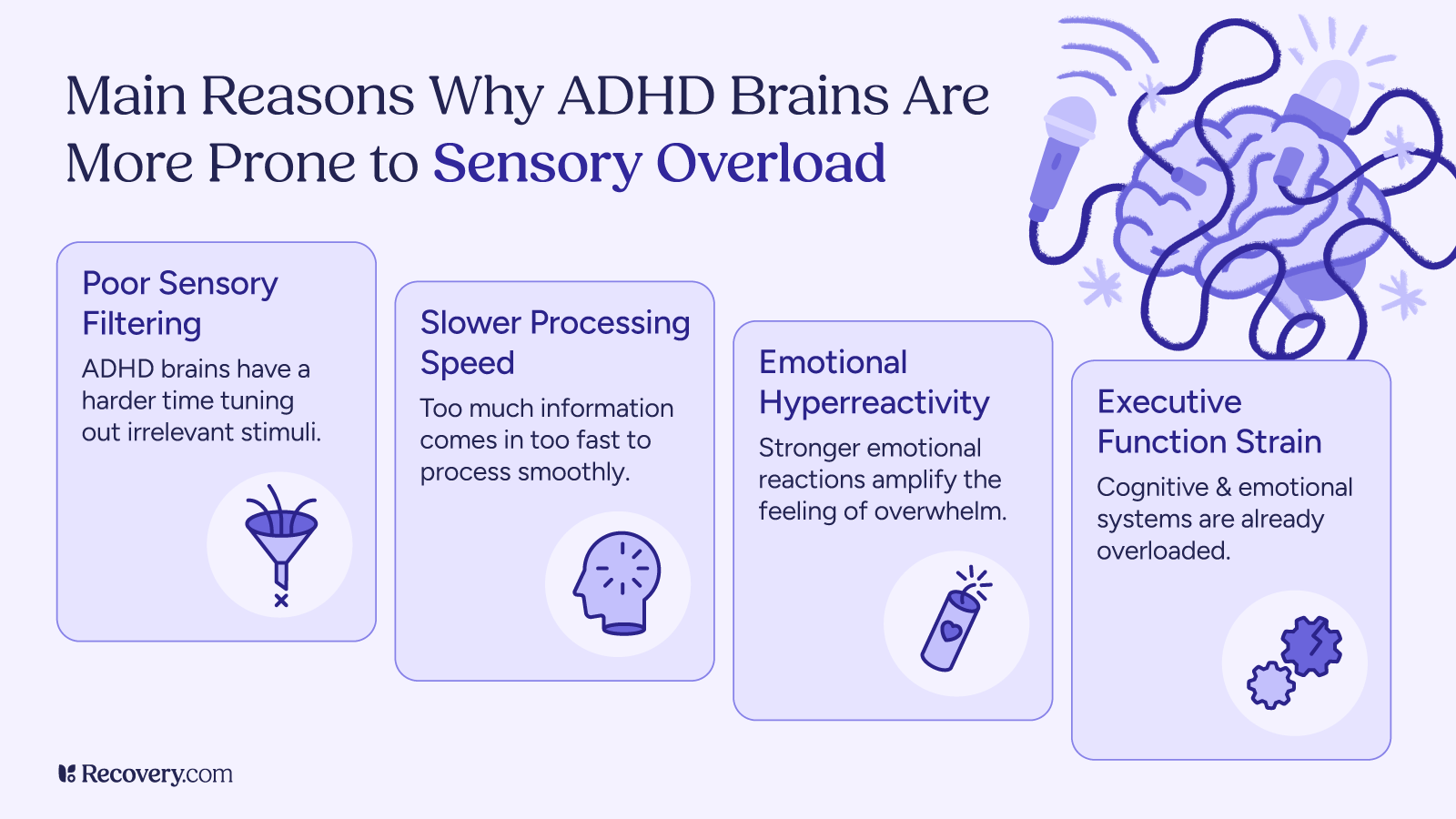
What Leads to Sensory Overload?
Sensory overload in individuals with ADHD can be attributed to several causes, many of which relate to the way their brains process sensory information. Here are some key factors, explained in an accessible way:
- Increased Hypersensitivity: People with ADHD often have a heightened sensory sensitivity to sensory input, meaning their brains are more reactive to stimuli like sounds, lights, and textures.7 For example, while a typical busy environment might feel just lively to some, an individual with ADHD may perceive it as chaotic and overwhelming, leading to discomfort and difficulty focusing.
- Difficulties with Filtering Information: The brain’s ability to filter out irrelevant sensory information is less efficient in those with ADHD. This means they may struggle to tune out background noise or visual distractions. Imagine trying to watch a movie while someone is talking loudly in the background. For someone with ADHD, the distractions can be hard to ignore, making it difficult to concentrate on the movie.
- Imbalances in Neurotransmitters: Neurotransmitters are chemicals in the brain that help transmit signals between nerve cells. In individuals with ADHD, there can be imbalances, particularly with dopamine and norepinephrine, which play roles in attention and arousal.8 When the brain struggles to manage these chemicals effectively, it can lead to a state of sensory overload, as the individual may react more strongly to stimuli that would typically be manageable.
- Co-Existing Conditions: Many individuals with ADHD also experience other conditions, such as anxiety or sensory processing disorder. These co-occurring conditions can exacerbate sensory overload symptoms. For instance, someone with both ADHD and anxiety might feel even more overwhelmed in bustling environments, as their anxiety amplifies their reaction to sensory inputs.9
- Environmental Factors: The environments in which individuals with ADHD find themselves can significantly affect sensory overload. Bright lights, loud noises, or crowded spaces can trigger an intense sensory reaction. Think about a busy supermarket on a Saturday afternoon; the combination of bright lights, loud announcements, and crowded aisles can create a sensory overload experience for someone with ADHD.
By understanding these causes, we can better support individuals with ADHD in managing sensory overload and creating environments that are more accommodating to their needs.
The Sensory Overload Experience for Those with Higher Functioning ADHD
High-functioning ADHD often presents differently than traditional forms of the disorder, with individuals able to maintain various levels of functionality in their daily lives. However, they still experience symptoms that can impact their social, academic, and professional functioning and may benefit from medical advice or treatment.
Here are some common symptoms of high-functioning ADHD, along with relatable examples:
- Chronic Disorganization: Frequently misplacing items (like keys or important documents) and struggling to maintain an organized workspace or living area, leading to frustration in daily routines.
- Procrastination: Putting off important tasks until the last minute, causing stress and a rush to complete work that could have been managed more smoothly over time.
- Difficulty Focusing on Tasks: Starting a project enthusiastically but becoming easily distracted by background noises or even by the urge to check social media, preventing completion of the task.
- Impulsivity in Social Situations: Interrupting friends during conversations or blurting out thoughts without considering the social context, which can lead to misunderstandings.
- Emotional Dysregulation: Experiencing intense emotional reactions, such as anger or sadness, over relatively minor issues, which may be perplexing to friends or family.
- Restlessness: Feeling the need to constantly move or fidget, even in situations where it’s not appropriate to do so, like tapping a foot during a meeting or shifting in a chair.
- Difficulty Following Through on Commitments: Agreeing to help a friend but forgetting about the commitment, leading to guilt and potential strain in the friendship.
- Hyperfocus: Becoming so engrossed in a hobby or a special interest that hours can pass unnoticed, resulting in missed obligations or deadlines.
- Sensitivity to Feedback: Taking constructive criticism very personally, leading to feelings of inadequacy or frustration, even when the feedback is meant to be helpful.
Understanding these symptoms can help individuals with high-functioning ADHD identify and address their challenges more effectively, leading to improved self-awareness and strategies for managing their daily lives.
What are some of the most overlooked environmental or emotional triggers that contribute to sensory overload in adults with ADHD?

Dual Diagnosis: ADHD and Substance Use Disorders
Sensory overload can be particularly challenging for individuals who are dually diagnosed with Attention Deficit Hyperactivity Disorder (ADHD) and a substance use or alcohol use disorder. The interplay between these conditions can exacerbate the experience of sensory overload and create a complex set of challenges.
Here’s how this phenomenon affects individuals with such dual diagnoses:
- Increased Sensitivity to Stimuli: Individuals with ADHD often exhibit heightened sensitivity to sensory stimuli.10 This can be intensified when coupled with a substance use disorder, as substances may alter sensory perception, making environments feel more chaotic or overwhelming. For example, someone in recovery from alcohol use disorder might find bright lights, loud noises, or other sensory triggers, particularly jarring, leading to feelings of anxiety or distress.
- Impaired Coping Mechanisms: Substance use may initially provide the individual with a way to escape from overwhelming sensory experiences. However, over time, reliance on substances can hinder the development of effective coping strategies. When not using substances, the individual may struggle to handle sensory input due to a lack of established coping mechanisms.
- Emotional Dysregulation: ADHD is often linked to emotional dysregulation, where individuals may have difficulty managing their emotions and reactions to stress. When combined with the effects of substance use, which can further impair judgment and emotional control, sensory overload can lead to emotional outbursts and/or heightened irritability, aggression, or feelings of helplessness in response to overwhelming stimuli.
- Triggers and Cravings: Certain sensory environments can serve as triggers for cravings or relapse in individuals in recovery. For instance, loud music or crowded spaces might remind someone of experiences associated with substance use, leading to uncomfortable feelings or a desire to self-medicate with drugs or alcohol.
- Social Challenges: Social situations, which can be inherently sensory-rich, may pose additional hurdles for individuals with this dual diagnosis. The combination of ADHD-related impulsivity and the effects of substance use can lead to social anxiety or uncomfortable interactions, making it difficult to navigate typical social environments without feeling overwhelmed.11
Despite these challenges, individuals with a dual diagnosis can implement tailored strategies, such as the following to manage sensory overload effectively:
Structured Environments: Create calm, predictable spaces at home or work that minimize sensory distractions. Using soft lighting and comfortable textures can help reduce overwhelming feelings.
Mindfulness Techniques: Mindfulness and grounding exercises can be particularly beneficial for those experiencing sensory overload. Techniques such as deep breathing or focusing on one sensory aspect at a time can help regain control.
Professional Support: Engaging with therapists or support groups specializing in dual diagnosis (i.e., Dual Recovery Anonymous/DRA) can provide valuable coping strategies and emotional support. Cognitive-behavioral therapy (CBT) can be particularly effective in addressing both ADHD and substance use issues.
Gradual Exposure: Gradually exposing oneself to social situations or environments that may be overwhelming can help build tolerance and reduce anxiety over time. It may also help to visit these places during less busy times.
Routine Breaks: Scheduling regular breaks during activities or work can help manage sensory input effectively, allowing time to recharge and refocus.
Understanding the complexities of sensory overload in individuals with both ADHD and substance use disorder is crucial for creating effective interventions and support systems. By fostering awareness and employing adaptive strategies, individuals can work toward improving their quality of life while navigating the challenges posed by both conditions.
Effective Coping Skills
Coping skills play a crucial role in managing sensory overload and hypersensitivity for individuals diagnosed with ADHD. These skills provide strategies for recognizing and regulating sensory input, enabling individuals to navigate overwhelming environments more effectively.
Here’s a list of effective coping skills that individuals diagnosed with ADHD can use to minimize sensory overload:12
- Create a Calm Space: Designate a quiet area at home where you can retreat when feeling overwhelmed. Use soft lighting, calming colors, and minimal decorations to reduce distractions.
- Use Noise-Canceling Headphones: Invest in good-quality headphones to block out distracting sounds. Listening to calming music or white noise can also help create a soothing auditory environment.
- Practice Mindfulness and Deep Breathing: Engage in mindfulness exercises and deep breathing techniques to center your thoughts and reduce anxiety during overwhelming situations.
- Establish Routine Breaks: Schedule regular breaks during tasks to step away from sensory input. Use this time to engage in a short walk, stretching, or a brief relaxation exercise.
- Limit Multitasking: Focus on one task at a time instead of juggling multiple activities. This helps reduce cognitive load and allows for better concentration.
- Use Visual Tools: Utilize tools like planners, to-do lists, or visual timers to stay organized and manage tasks more effectively, reducing the mental noise associated with forgetfulness.
- Gradual Exposure: If certain environments are overwhelming, consider gradual exposure. Spend short periods in busy settings and gradually increase your time as you become more comfortable.
- Engage in Sensory Grounding Techniques: Practicing grounding techniques, such as feeling a textured item or aromatherapy, can help refocus your attention and soothe sensory overload.
- Communicate Preferences: Inform family, friends, or coworkers about your sensory sensitivities, and advocate for environments that accommodate your needs, such as quieter meeting spaces.
- Stay Hydrated and Well-Nourished: Ensure you are drinking enough water and eating balanced meals. Dehydration or poor nutrition can heighten sensitivity to sensory input.
- Develop a Personal Sensory Diet: Create a sensory diet that includes a variety of activities tailored to your needs, such as physical exercise, creative pursuits, or calming hobbies that help regulate sensory input.
Implementing these coping skills can empower individuals with ADHD to take control of their sensory experiences, minimize feelings of overload, and enhance their overall quality of life.
What advice would you give to someone navigating both ADHD and a co-occurring condition like anxiety or substance use, especially when it comes to managing overwhelming sensory input?

Medication Options
Medications for ADHD, primarily stimulant and non-stimulant options, can play a significant role in alleviating sensory issues and processing challenges associated with the condition. Stimulants, such as methylphenidate (i.e., Ritalin, Concerta) and amphetamine-based (i.e., Adderall, Vyvanse) medications, work by increasing levels of dopamine and norepinephrine in the brain, enhancing attention, focus, and impulse control.
By improving these cognitive functions, individuals may find it easier to filter and manage sensory input, reducing feelings of overwhelm. Non-stimulant medications, like atomoxetine, can also assist with attention and impulse regulation, contributing to improved emotional stability and social interactions. Ultimately, medication can serve as a valuable component in a comprehensive treatment plan aimed at addressing both ADHD symptoms and sensory processing difficulties.
The Bright Side of ADHD
While ADHD can present challenges, many individuals who effectively manage their symptoms find that they can enjoy several unique benefits. Here are some potential advantages of having ADHD when it is well-controlled:
- Creativity and Innovation: Individuals with ADHD often think outside the box and are capable of coming up with creative solutions to problems. Their ability to connect unrelated ideas can lead to innovative thinking and unique perspectives.
- Hyperfocus Ability: One of the hallmark traits of ADHD is the capacity for hyperfocus—becoming intensely absorbed in tasks that are stimulating or interesting. This can lead to high productivity levels when working on projects or pursuits that capture one’s attention.
- High Energy Levels: Many individuals with ADHD possess abundant energy, which can be channeled into productive activities. When managed well, this energy can enhance performance in both work and hobbies.
- Adaptability and Flexibility: Individuals with ADHD often learn to adapt quickly to changing situations. Their experiences in navigating diverse environments can foster a sense of flexibility that is beneficial in fast-paced careers.
- Strong Problem-Solving Skills: The ability to see the bigger picture and navigate complexities can lead to exceptional problem-solving skills. Many individuals with ADHD excel in high-pressure situations where quick thinking is required.
- Passion and Enthusiasm: People with ADHD often approach their interests and passions with great enthusiasm. This can infectious energy can inspire and motivate others in collaborative settings.
- Resilience: Overcoming the challenges posed by ADHD can develop strong resilience and perseverance. Many individuals become adept at facing obstacles and finding creative ways to overcome themwhat-is-sensory-overload.
- Outstanding People Skills: Many individuals with ADHD are outgoing and enjoy engaging with others. They can form strong interpersonal connections and excel in social situations, often being perceived as charismatic or engaging.
- Enhanced Multitasking Abilities: While multitasking can be challenging, people with ADHD often thrive on switching between tasks, enabling them to manage various projects simultaneously when it fits their work style.
- Unique Learning Styles: Individuals with ADHD may have unconventional learning styles that can foster creativity and a different approach to acquiring knowledge. This adaptability can lead to innovative ways of thinking and working.
When individuals with ADHD effectively harness and manage their symptoms through strategies like mindfulness, organizational tools, and support systems, they can turn these potential advantages into strengths in both their personal and professional lives.
Conclusion
If you or someone you know is grappling with sensory overload related to ADHD, seeking support is essential. This can be achieved through therapy, where professionals can offer tailored strategies and coping mechanisms. Connecting with support groups or community resources can also provide valuable insights and camaraderie. Developing skills such as mindfulness, organizational techniques, and creating a structured environment can help mitigate the effects of sensory overload.
Remember, while the challenges associated with ADHD and sensory overload can be daunting, there is hope for growth and improvement.13 With the right tools and support, individuals can learn to navigate their environments more comfortably, embracing their unique strengths and perspectives.
Mental health struggles can feel isolating, but compassionate care is within reach. Browse our comprehensive list of inpatient mental health facilities and residential treatment centers for ADHD and more. Healing is possible; find mental health help for yourself or a loved one today.
FAQs
-
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). https://doi.org/10.1176/appi.books.9780890425787
-
Lane, S. J., & Reynolds, S. (2019). Sensory Over-Responsivity as an Added Dimension in ADHD. Frontiers in integrative neuroscience, 13, 40. https://doi.org/10.3389/fnint.2019.00040
-
https://psychiatryinvestigation.org/journal/view.php?doi=10.4306/pi.2011.8.2.89
-
Bijlenga, D., Tjon-Ka-Jie, J. Y. M., Schuijers, F., & Kooij, J. J. S. (2017). Atypical sensory profiles as core features of adult ADHD, irrespective of autistic symptoms. European Psychiatry, 43, 51–57. doi:10.1016/j.eurpsy.2017.02.481
-
Ranjbar-Slamloo, Y., & Fazlali, Z. (2020). Dopamine and noradrenaline in the brain; overlapping or dissociate functions? Frontiers in Integrative Neuroscience, 13, Article 40. https://doi.org/10.3389/fnint.2019.00040
-
Masi, G., Liboni, F., Lin, P. I., & Pfanner, C. (2025). Emotional dysregulation and comorbidities in ADHD across the lifespan. Journal of the American Academy of Child & Adolescent Psychiatry. Advance online publication. https://doi.org/10.1016/j.jaac.2024.03.010
-
Masi, G., Liboni, F., Lin, P. I., & Pfanner, C. (2025). Emotional dysregulation and comorbidities in ADHD across the lifespan. Journal of the American Academy of Child & Adolescent Psychiatry. Advance online publication. https://doi.org/10.1016/j.jaac.2024.03.010
-
Bush, G. (2010). Attention‐deficit/hyperactivity disorder and attention networks. Human Brain Mapping, 31(4), 476–485. https://doi.org/10.1002/hbm.21058
-
Breaux, R. P., Langberg, J. M., & Becker, S. P. (2023). Coping strategies mediate the relation between executive functioning deficits and depressive symptoms in adolescents with ADHD. Journal of Health Psychology. Advance online publication. https://doi.org/10.1177/20438087231204168
-
Ormston, T., & Heidari, E. (2024). Attention deficit hyperactivity disorder. In StatPearls. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK563136/
-
Hofmann, S. G., & Bitran, S. (2007). Sensory-processing sensitivity in social anxiety disorder: relationship to harm avoidance and diagnostic subtypes. Journal of anxiety disorders, 21(7), 944–954. https://doi.org/10.1016/j.janxdis.2006.12.003
-
Martel, M. M., Nikolas, M., Jernigan, K., Friderici, K., & Nigg, J. T. (2005). Executive function in adolescents with ADHD. Personality and Individual Differences, 39(3), 451–461. https://doi.org/10.1016/j.paid.2004.12.007
-
Lane, S. J., & Reynolds, S. (2019). Sensory Over-Responsivity as an Added Dimension in ADHD. Frontiers in integrative neuroscience, 13, 40. https://doi.org/10.3389/fnint.2019.00040
Our Promise
How Is Recovery.com Different?
We believe everyone deserves access to accurate, unbiased information about mental health and recovery. That’s why we have a comprehensive set of treatment providers and don't charge for inclusion. Any center that meets our criteria can list for free. We do not and have never accepted fees for referring someone to a particular center. Providers who advertise with us must be verified by our Research Team and we clearly mark their status as advertisers.
Our goal is to help you choose the best path for your recovery. That begins with information you can trust.











