How Can I Pay for Treatment? 6 Ways to Afford Mental Health and Addiction Care



Hannah is a holistic wellness writer who explores post-traumatic growth and the mind-body connection through her work for various health and wellness platforms. She is also a licensed massage therapist who has contributed meditations, essays, and blog posts to apps and websites focused on mental health and fitness.

Dr. Mala, is the Chief Clinical Officer at Recovery.com, where she develops impartial and informative resources for people seeking addiction and mental health treatment.




Hannah is a holistic wellness writer who explores post-traumatic growth and the mind-body connection through her work for various health and wellness platforms. She is also a licensed massage therapist who has contributed meditations, essays, and blog posts to apps and websites focused on mental health and fitness.

Dr. Mala, is the Chief Clinical Officer at Recovery.com, where she develops impartial and informative resources for people seeking addiction and mental health treatment.
Table of Contents
- Understanding What Affects Treatment Costs
- 1. Use Your Insurance Benefits
- 2. Understand Treatment Costs by Level of Care
- 3. Know How to Access Out-of-Network Providers
- 4. Ask About Payment Plans and Sliding Scales
- 5. Apply for Grants, Scholarships, and State Funding
- 6. Get Help From an Insurance Advocate or Case Manager
When you're ready to get help for addiction, one question often looms large: How am I going to pay for this?
The truth is that treatment is an investment in your health and future, and it can be expensive. But cost doesn't have to be a barrier. From maximizing your insurance benefits to finding grants and payment plans, there are more ways to afford care than most people realize.
We'll walk you through the most common payment options, help you understand what to expect at each level of care, and show you how to find financial support that fits your situation. If you're ready to start your recovery, you may have more options than you think.

Understanding What Affects Treatment Costs
There isn't a fixed price for addiction treatment. Instead, a variety of elements can affect the cost of your care. The cost of rehab varies depending on several factors and is typically higher for inpatient or residential programs, where you reside at the facility 24/7.
The cost for alcohol or drug rehab usually depends on:
- Facility location
- Level of care
- Private vs. shared accommodations
- Services offered
- Medications used
- Amenities offered (e.g., equine therapy, yoga, art therapy)
- Insurance coverage
- How long treatment lasts (e.g., 28 to 30 days, 60 days, 90 days)
Putting off getting treatment due to monetary concerns can be dangerous, as allowing an addiction to continue without treatment can cause long-term health problems and even death. Learning more about addiction treatment costs can help you connect to treatment that can ultimately save your life.
1. Use Your Insurance Benefits
Most health insurance plans in the U.S. do cover mental health and addiction treatment.1 Since the Affordable Care Act (ACA) was passed, insurance companies are required to treat mental health services the same way they treat medical services. This means your coverage for therapy, rehab, or other treatment can't be more restrictive than coverage for things like surgery or hospital stays.
However, insurance companies decide what they think is "medically necessary," which means they might say no to treatment even when your doctor recommends it.2 Your insurance may cover some or all of your treatment costs; eligibility depends on your plan and whether they approve your care.
Most private rehab centers accept insurance and offer multiple payment options to help make treatment accessible. Some facilities also accept Medicare or Medicaid, though coverage can vary by state and provider.
How to Verify Benefits and Understand Behavioral Health Coverage
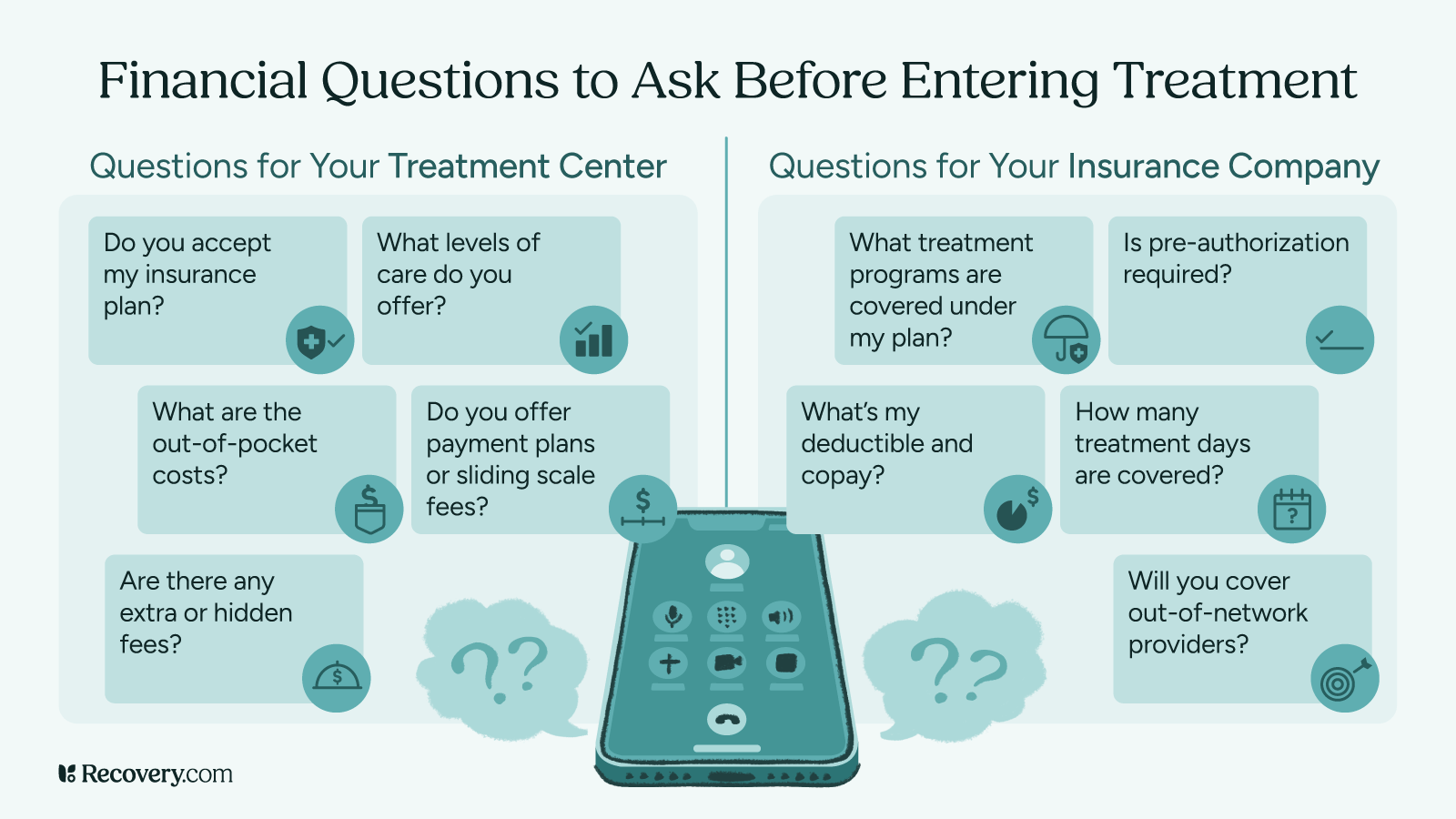
Before starting treatment, call your insurance company directly to understand your benefits. A customer service representative can walk you through your coverage details and help you understand what you'll pay out of pocket.
Here are the key questions to ask your insurance provider:
- What treatment programs does my policy cover?
- Does my plan cover the full spectrum of care (detox, rehab, and continuing care)?
- How much will I need to pay out of pocket?
- What will my deductible and copayment be?
- How many days of treatment are covered?
- Will my insurance cover prescribed medications?
- Does my plan cover out-of-network treatment centers?
You can also ask your treatment center's admissions team to help verify your benefits. Many centers have staff who specialize in insurance and can help you understand your coverage before you start treatment.
2. Understand Treatment Costs by Level of Care
The cost of your treatment will also depend on how intensive it is. Components of treatment like levels of care and specific amenities can all impact your overall cost of care. Here's what you can expect for detox, inpatient, outpatient, and ongoing therapy:
Medical Detox
Detoxification, or detox, is a set of interventions to help you manage drug and alcohol withdrawal symptoms. When conducted in a professional setting, detox offers you 24-hour medical observation and support to help you safely and comfortably withdraw from substances.
Some inpatient rehabs have detox facilities onsite. In other cases, detox is handled at a separate facility. In either case, medical detox is usually an additional cost above and beyond the price of your residential treatment program.
Medical detox costs vary widely based on the level of care you need.3 Standard inpatient detox typically costs $250–$800 per day, while supervised detox with 24/7 medical care runs $500–$650 per day. Outpatient detox costs has lower overall costs since you go home each night.
Keep in mind that these are general ranges. Your actual costs will depend on your insurance coverage, the specific facility you choose, and your individual needs while in treatment.
Inpatient (Residential) Treatment
Inpatient rehab, which is sometimes called residential treatment, is a treatment setting where you live for the duration of your treatment while participating in an alcohol or drug rehabilitation program. This level of addiction treatment is usually recommended for people who have co-occurring disorders, have experienced chronic relapse, or need a more intensive level of care due to a severe addiction.
Inpatient treatment is typically more expensive than other levels of care because you will reside at the facility and have access to a team of treatment professionals 24/7. The exact cost of inpatient rehab will depend on several factors, including the offered amenities at your facility, your treatment location, prescribed medications, and the length of your stay.
In the U.S., most 30-day programs at private facilities cost between $25,000 to $50,000 per month, though the prices of residential rehab programs can range from under $10,000 to upwards of $80,000. If you travel to countries with lower costs of living, such as Thailand or India, programs often cost under $15,000 per month.
Outpatient Programs
Outpatient treatment lets you live at home while attending therapy and support sessions. This category includes standard outpatient programs, intensive outpatient programs (IOPs), and partial hospitalization programs (PHPs).
Your costs will depend on which type of program you choose and how often you attend. Outpatient rehab generally costs less than inpatient treatment, but IOPs and PHPs are more intensive and therefore more expensive than standard outpatient care.
Intensive Outpatient Programs
Intensive outpatient programs (IOPs) in the U.S. range from $3,500 to over $10,000 depending on the length and number of sessions. Individual therapy with a private practitioner typically costs $65 to $250 per hour.
Partial Hospitalization Programs (PHPs)
These programs, known as PHPs, offer more intensive care than outpatient but allow you to go home each night, typically cost $3,500 to upwards of $10,000 at private facilities.

3. Know How to Access Out-of-Network Providers
Sometimes the treatment program you really want to attend is not in your insurance network. This doesn't mean you can't access care there, but it does mean you'll likely pay more out of pocket.
Options If Your Preferred Provider Isn't Covered
If your preferred treatment center is out-of-network, you have several options. First, ask your insurance company if they offer any out-of-network benefits. Some plans will still cover a percentage of costs, even at non-network treatment facilities.
You can also ask the treatment center about their self-pay rates or cash pay discounts. Some centers have relationships with financing companies that can help you create affordable payment plans.
Another option is to ask your insurance company about single-case agreements. In some situations, especially when in-network options are limited, insurance companies will agree to cover an out-of-network health care provider at in-network rates.
4. Ask About Payment Plans and Sliding Scales
Treatment centers understand that cost can be a barrier to care. That's why most facilities offer flexible payment options to help make treatment more affordable.
What to Ask When Money Is Tight
Figuring out how to pay for rehab can feel overwhelming and stressful, but it doesn't have to be. If you're concerned about costs, be upfront with your rehab's admissions staff about your financial situation. Often, facilities can work with you to create a payment plan that fits your budget. Ask about:
- Interest-free payment plans that let you spread costs over several months
- Sliding-scale fees based on your income
- Discounts for paying your balance in full upfront
- Work-trade arrangements where you can reduce costs by helping with facility operations
- Scholarships or hardship funds they might have available
Don't be afraid to negotiate. Treatment centers want to help people get the care they need, and some have flexibility in their pricing. The worst they can say is no, but you might be surprised by what options are available.
5. Apply for Grants, Scholarships, and State Funding
Beyond insurance and payment plans, there are other sources of funding that can help cover treatment costs. If you are uninsured, know that you can still get the help you need. Paying privately, getting financial assistance from friends or family, applying for government scholarships to cover your drug rehab cost, or asking if your facility offers assistance can all be workable options.
Public Resources and Nonprofit Support
Many states offer funding for addiction and mental health care through grants and public programs. Contact your state's department of health or substance abuse agency to learn about programs in your area. These programs often have income requirements and may have waiting lists, but they can provide significant financial assistance.
Some nonprofit organizations also offer substance use disorder treatment scholarships. These might be available through professional associations, religious organizations, or foundations focused on mental illness and substance use disorders. Search online for "addiction treatment scholarships" or "mental health treatment grants" in your area.
If you're a veteran, you may qualify for treatment through the VA healthcare system.4 Students might find resources through their college or university counseling centers, which often provide low-cost or free behavioral health services.
Always be wary of addiction treatment scams and rehab-owned referral sites posing as objective resources when searching for help online. Learn more in our article on how to avoid common addiction treatment center scams.
6. Get Help From an Insurance Advocate or Case Manager
Navigating insurance and treatment costs can be overwhelming, especially when you're already facing a crisis. But luckily, you don't have to figure it all out alone.
How Professionals Can Help Reduce Financial Stress
Many treatment centers employ insurance specialists or case managers who can help you understand your benefits and find ways to make treatment affordable. These professionals know the ins and outs of insurance coverage and can advocate on your behalf.
If your insurance claim gets denied, these advocates can help you appeal the decision. You have the right to appeal any denied claim through your insurance company's internal review process, or through an independent external review if needed.
Some community-based organizations also have independent patient advocates or social workers who specialize in helping people access health care. Your doctor, local health department, or a reputable helpline can help you find these resources in your area.
Start Your Recovery Journey
If you’re ready to find addiction treatment for yourself or a loved one, we’re here to help. Browse top medical detox centers in the US, inpatient addiction treatment facilities, aftercare options, and more to start on the path to recovery. You can search for rehab by insurance carrier, location, amenities, and more for free.
Don’t wait. Get help today.
-
HealthCare.gov. Mental Health and Substance Abuse Health Coverage Options. https://www.healthcare.gov/coverage/mental-health-substance-abuse-coverage/
-
Waldman, Annie. Insurers Can Restrict Mental Health Care. What Laws Protect Patients in Your State? NPR, 27 Aug. 2024. NPR. https://www.npr.org/sections/shots-health-news/2024/08/23/nx-s1-5084256/insurance-mental-health-care-coverage-legal-protection
-
NCDAS. “Average Cost of Drug Rehab [2023]: By Type, State & More. https://drugabusestatistics.org/cost-of-rehab/
-
Peter, S., Halverson, T., Blakey, S., Pugh, M.J., Beckham, J.C., Calhoun, P.S., Kimbrel, N.A. (2022, July 4). The Veterans Health Administration's Integrated Model of Care Increases Accessibility and Delivery of Mental Health Services. https://pmc.ncbi.nlm.nih.gov/articles/PMC9810760/
Our Promise
How Is Recovery.com Different?
We believe everyone deserves access to accurate, unbiased information about mental health and recovery. That’s why we have a comprehensive set of treatment providers and don't charge for inclusion. Any center that meets our criteria can list for free. We do not and have never accepted fees for referring someone to a particular center. Providers who advertise with us must be verified by our Research Team and we clearly mark their status as advertisers.
Our goal is to help you choose the best path for your recovery. That begins with information you can trust.









