Xanax Withdrawal Symptoms: What to Expect and When to Get Help



Hannah is a holistic wellness writer who explores post-traumatic growth and the mind-body connection through her work for various health and wellness platforms. She is also a licensed massage therapist who has contributed meditations, essays, and blog posts to apps and websites focused on mental health and fitness.

Dr. Mala, is the Chief Clinical Officer at Recovery.com, where she develops impartial and informative resources for people seeking addiction and mental health treatment.




Hannah is a holistic wellness writer who explores post-traumatic growth and the mind-body connection through her work for various health and wellness platforms. She is also a licensed massage therapist who has contributed meditations, essays, and blog posts to apps and websites focused on mental health and fitness.

Dr. Mala, is the Chief Clinical Officer at Recovery.com, where she develops impartial and informative resources for people seeking addiction and mental health treatment.
Table of Contents
- What Is Xanax and Why Does Your Body Become Dependent on It?
- What Happens During Xanax Withdrawal?
- Common Xanax Withdrawal Symptoms
- Serious Withdrawal Symptoms: When to Get Immediate Help
- When Will I Feel Better? The Xanax Withdrawal Timeline
- Factors That Affect Your Withdrawal Experience
- Xanax Detox and Recovery: Find Help for the Journey Ahead
If you take Xanax, it’s important to understand how your body can become dependent on it and what happens when you stop. Xanax (alprazolam) is a medication doctors often prescribe for certain mental health conditions like anxiety and panic disorders.
While it can help manage severe anxiety in the short term, if you continue taking Xanax, it doesn’t take long for your brain to start relying on it. When you cut back or stop taking Xanax, your body needs time to adjust—and that’s when withdrawal symptoms can show up.
Xanax withdrawal can feel anywhere from uncomfortable (like a bad flu) to very tough to handle, but knowing what to expect can help you prepare and get through it safely. Let’s look at what happens during withdrawal, the symptoms you might experience, and how getting the right support can make all the difference.
IMPORTANT NOTE: Never attempt Xanax detox without medical support.Withdrawing from Xanax on your own can be dangerous and potentially life-threatening, with risks including seizures and psychosis in severe cases.
When you’re ready to stop taking Xanax, always consult with a healthcare provider first, never stop “cold turkey,” and follow a medically supervised tapering schedule that gradually reduces your dose over time. Even if you’ve been taking Xanax exactly as prescribed, your body may have developed a physical dependence that requires careful management during discontinuation.
Medical supervision ensures you can withdraw safely while managing symptoms effectively, providing tools and medications that make the process much more comfortable and significantly safer than attempting it alone.
What Is Xanax and Why Does Your Body Become Dependent on It?
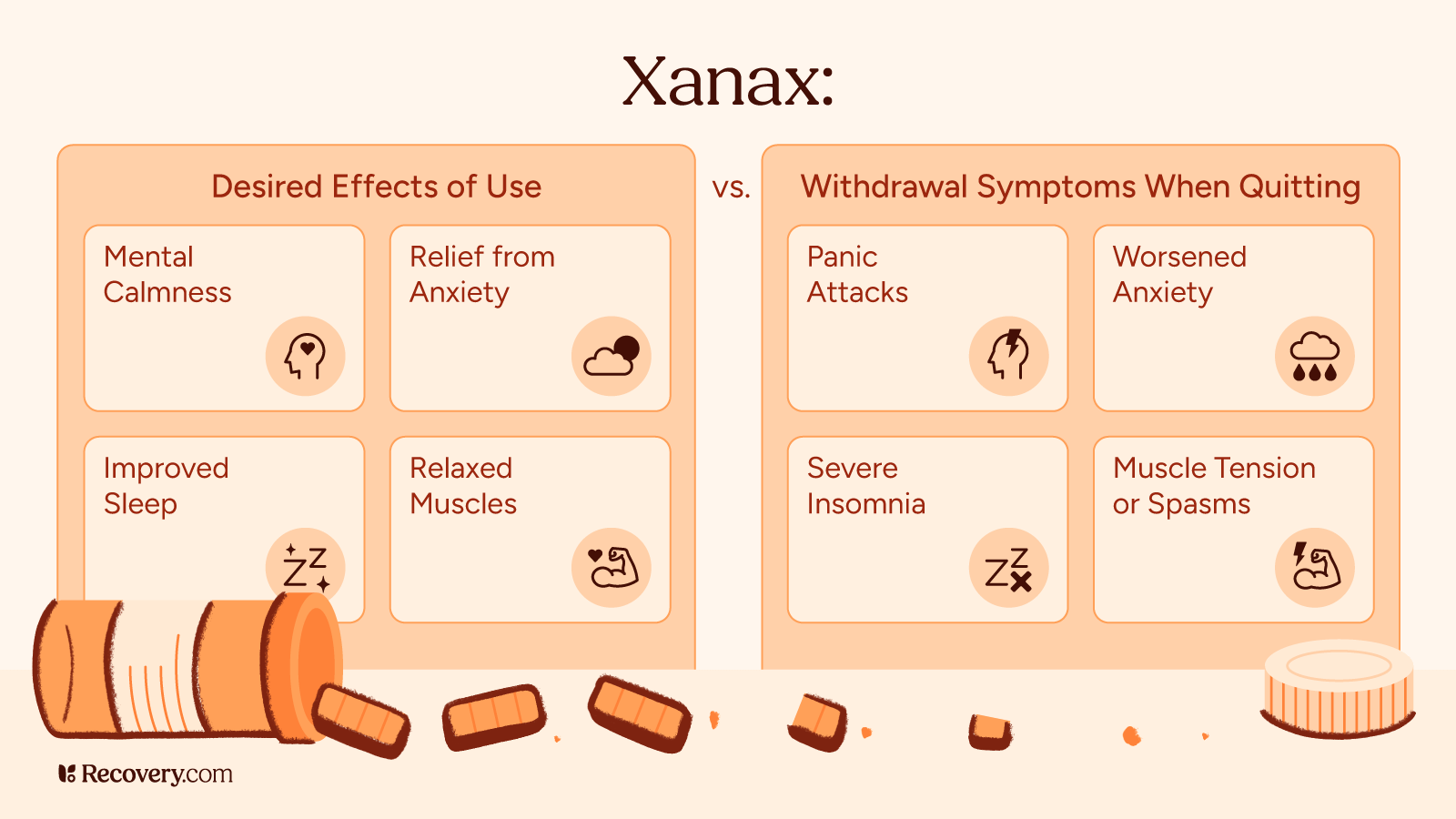
Xanax belongs to a family of medications called benzodiazepines (or “benzos” for short).1 These medications work by boosting a natural calming chemical in your brain called GABA. When you take Xanax, it slows down your overactive brain, which helps reduce anxiety and panic attacks. That’s why it can make you feel relaxed, sleepy, and less bothered by stress.
Physical Dependence: When Your Body Expects Xanax
Because your brain is designed to adapt quickly, it quickly gets used to having Xanax around. After just a few weeks of regular use, your brain starts making less of its own calming chemicals because it’s counting on the medication to do the job instead.
Doctors call this dependence. It means your body has gotten used to functioning with Xanax in your system.
You can become dependent on Xanax even if you’re taking it exactly as prescribed.2 Physiological dependence can happen in as little as 3-4 weeks of regular use, even at normal doses. That’s why doctors usually only recommend Xanax for short periods. The more you take and the longer you use it, the more your body comes to rely on it.
Addiction: When Xanax Takes Control
Addiction is different from dependence. While dependence is about your body physically adapting to the drug, addiction involves behaviors like taking more than prescribed, seeing multiple doctors to get extra prescriptions, or continuing to use Xanax despite the problems it’s causing in your life.
Not everyone who becomes dependent develops a substance use disorder, but the longer you take Xanax, the more your risk of addiction increases.3
What Happens During Xanax Withdrawal?
When you stop taking Xanax, your brain needs to remember how to work on its own again. During this adjustment period, you might feel uncomfortable as your brain tries to restore its natural balance. That’s because your brain is relearning how to calm itself down without chemical help.
Common Xanax Withdrawal Symptoms
When you stop taking Xanax, you can experience several different kinds of symptoms. Here’s what you might feel and why it happens.
Physical Symptoms: How Your Body Reacts
The physical symptoms of Xanax withdrawal can feel a lot like having a bad flu or hangover.4 You might notice:
- Headaches, dizziness, or lightheadedness
- Fever or sweating more than usual
- Muscle spasms, aches, or shakiness
- Blurry vision or sensitivity to bright lights
- Nausea or stomach pain
- Having a hard time falling or staying asleep
- Heart palpitations or increased heart rate
- Higher blood pressure
Your body might feel extra sensitive during withdrawal, so everyday lights and sounds that normally wouldn’t bother you might suddenly feel too bright or too loud. This happens because Xanax is a central nervous system depressant, and without it, your nervous system has to work overtime to calm things down.
Mental and Emotional Symptoms: How Your Mind Reacts
Withdrawal can also affect how you feel emotionally and mentally. You might:
- Feel more anxious or have panic attacks (sometimes worse than before)
- Have mood swings or get irritated easily
- Feel mentally foggy or have trouble concentrating
- Feel down or hopeless
- Have racing thoughts
- Have strong cravings for Xanax
- Feel easily overwhelmed
You might notice that some withdrawal symptoms feel similar to the anxiety disorder you were taking Xanax for in the first place. This “rebound anxiety” is common and doesn’t mean your anxiety is getting worse permanently—it’s just part of the withdrawal process and will improve with time.
Serious Withdrawal Symptoms: When to Get Immediate Help
In some cases—especially after heavy or long-term use—Xanax withdrawal can cause more serious symptoms. If you experience any of these, you should seek medical attention right away:
- Seizures
- Seeing or hearing things that aren’t really there
- Severe confusion about where you are or what’s happening
- Losing touch with reality
These severe symptoms are more likely to happen if you stop Xanax suddenly (“cold turkey”) instead of gradually reducing your dose under a doctor’s guidance.5 This is why getting help from a medical professional during withdrawal is so important, especially if you’ve been taking higher doses or using Xanax for a long time.
When Will I Feel Better? The Xanax Withdrawal Timeline
No two people experience Xanax withdrawal exactly the same way, but there is a general pattern most people follow. Knowing what to expect and when can help you prepare and get the right support for your situation.
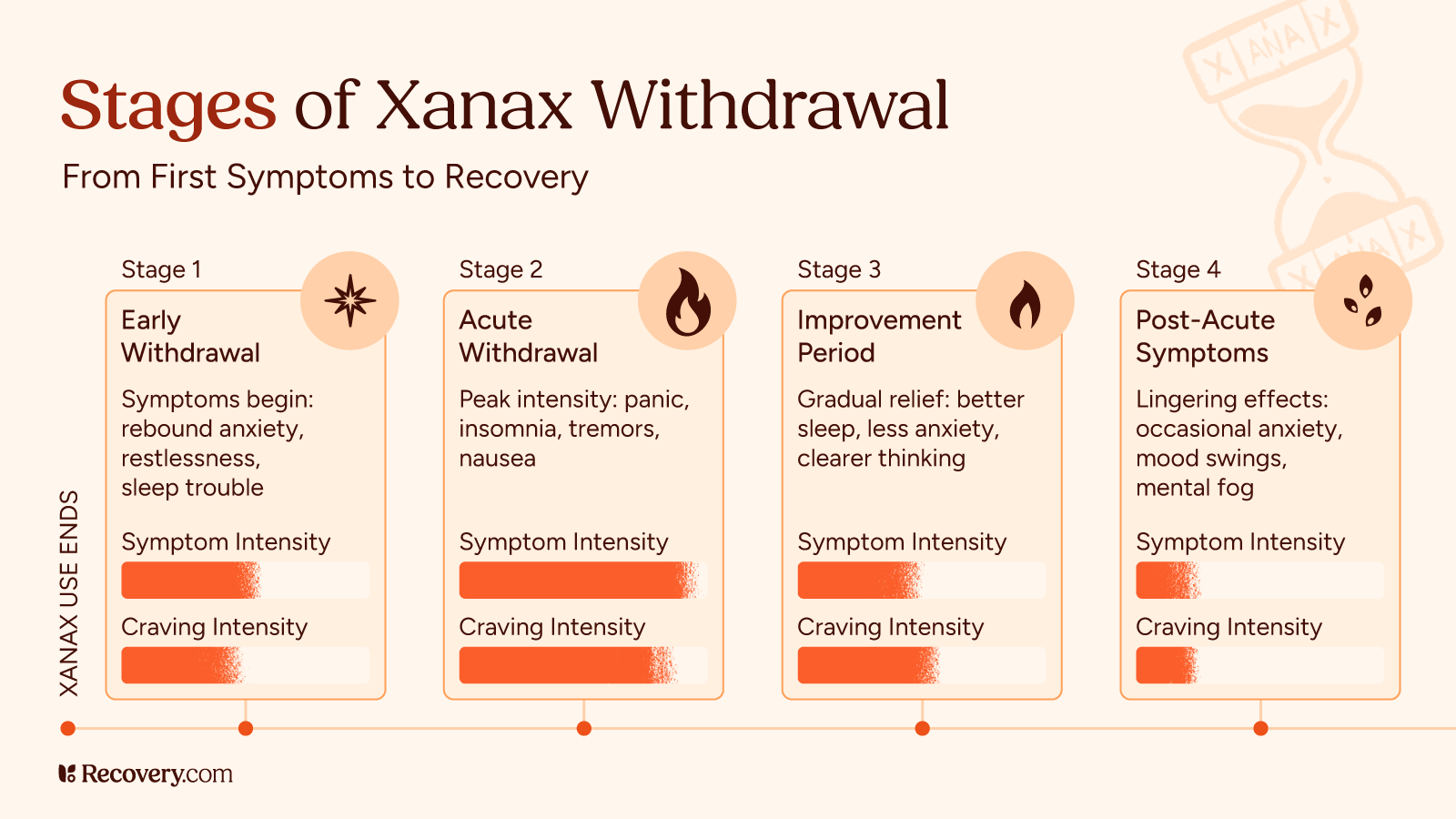
Early Withdrawal (1-4 Days After Your Last Dose)
Xanax withdrawal symptoms often kick in within 1-4 days after your last dose.6 Since Xanax is a short-acting benzodiazepine, it has a shorter half-life than many other benzos. This means you’ll likely notice symptoms starting sooner rather than later. During these first few days, you might experience:
- “Rebound” anxiety that might feel stronger than your original anxiety
- Trouble falling or staying asleep
- Feeling restless or on edge
- Irritability or mood changes
These early symptoms happen as your body first notices the absence of Xanax in your system.
Acute Withdrawal (Days 5-14)
The full-blown withdrawal syndrome typically lasts about 10-14 days. During this period, you might deal with:
- Increased anxiety and possible panic attacks
- Sleep disturbances and nightmares
- Physical symptoms like tremors, sweating, and nausea
- Difficulty concentrating or thinking clearly
- Muscle pain and stiffness
- Headaches and sensitivity to light
- In more severe cases, possible seizures (which is why medical supervision is crucial)7
This acute phase is when symptoms are typically most intense and when medical support is most important, especially if you’ve been on higher doses or taking Xanax long-term.
Improvement Period (After Week 2)
After the acute withdrawal phase, most people start to see gradual improvement. During this time, you might notice:
- Symptoms becoming less intense and more manageable
- Better sleep quality
- Decreasing anxiety levels
- More good days than hard ones
For some people, symptoms resolve completely within a few weeks. For others, some symptoms may persist longer.
The Long Haul: Months Later
Some people deal with lingering symptoms for months after stopping Xanax.8 Doctors call this post-acute withdrawal syndrome (PAWS). If this happens to you, you might experience:
- Occasional anxiety or panic attacks that come out of nowhere
- Nights where you just can’t sleep well
- Mood swings that seem to have no trigger
- Feeling mentally foggy or having trouble thinking clearly
The good news is these protracted withdrawal symptoms usually get milder and show up less often as time passes. For most people, they eventually go away completely, though it might take several months.
To learn more about long-term side effects, see our complete guide to post-acute withdrawal syndrome (PAWS) and how to manage these lingering symptoms.
Factors That Affect Your Withdrawal Experience
How long your withdrawal lasts and how severe it is depends on several factors:
- How much you were taking: Higher doses usually mean more severe withdrawal symptoms.
- How long you were taking it: Months or years of use means a longer recovery.
- How you stop: Gradually reducing your dose (tapering) under medical supervision causes fewer problems.
- Your personal health factors: Your age, overall health, and body chemistry matter.
- Past experiences: If you’ve gone through benzo withdrawal before, your body might be more sensitive.
This timeline is just a general roadmap. Your personal journey might look different, and that’s okay.
Xanax Detox and Recovery: Find Help for the Journey Ahead
Withdrawing from Xanax can be challenging, but with the right support and care, it’s a journey you can take on successfully. Keep in mind that the discomfort of withdrawal is temporary, and plenty of people have gone through this process and emerged stronger on the other side.
If you or your loved one is considering quitting Xanax, the first step is to speak with a healthcare professional. A qualified addiction medicine specialist can assess your situation and create a personalized treatment plan that may include inpatient or outpatient rehab and support groups. Don’t try to go through this alone—professional support is hugely important for your safety and comfort during withdrawal.
For help finding treatment options, search for specialized Xanax addiction treatment programs in your area. Recovery is possible, and support is available whenever you’re ready.
FAQs
-
1. Ait-Daoud, N., Hamby, A. S., Sharma, S., & Blevins, D. (2018). A Review of Alprazolam Use, Misuse, and Withdrawal. Journal of addiction medicine, 12(1), 4–10. https://doi.org/10.1097/ADM.0000000000000350
-
2. Kennedy, K. M., & O'Riordan, J. (2019). Prescribing benzodiazepines in general practice. The British journal of general practice : the journal of the Royal College of General Practitioners, 69(680), 152–153. https://doi.org/10.3399/bjgp19X701753
-
3. Sellers, E. M., Niciu, M. J., & Frazer, A. (2018). A review of alprazolam use, misuse, and withdrawal. Journal of Addiction Medicine, 12(1), 4–10. https://doi.org/10.1097/ADM.0000000000000361
-
4. Pétursson H. (1994). The benzodiazepine withdrawal syndrome. Addiction (Abingdon, England), 89(11), 1455–1459. https://doi.org/10.1111/j.1360-0443.1994.tb03743.x
-
5. McKenzie, R. R., Jr, Madadi, P., & Sharma, T. R. (2014). Alprazolam withdrawal delirium and brief reversible psychosis: a case report. The primary care companion for CNS disorders, 16(5), 10.4088/PCC.14l01668. https://doi.org/10.4088/PCC.14l01668
-
6. VandeVoort, J. L., & Castillo, E. M. (2023). Benzodiazepine Toxicity. In StatPearls. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK310652/
-
7. Hu X. (2011). Benzodiazepine withdrawal seizures and management. The Journal of the Oklahoma State Medical Association, 104(2), 62–65.
-
8. U.S. Food and Drug Administration. (2021). Xanax (alprazolam) [Prescribing information]. https://www.accessdata.fda.gov/drugsatfda_docs/label/2021/018276s058lbl.pdf
Our Promise
How Is Recovery.com Different?
We believe everyone deserves access to accurate, unbiased information about mental health and recovery. That’s why we have a comprehensive set of treatment providers and don't charge for inclusion. Any center that meets our criteria can list for free. We do not and have never accepted fees for referring someone to a particular center. Providers who advertise with us must be verified by our Research Team and we clearly mark their status as advertisers.
Our goal is to help you choose the best path for your recovery. That begins with information you can trust.