Tramadol Addiction: 4 Warning Signs and Effective Recovery Paths



Hannah is a holistic wellness writer who explores post-traumatic growth and the mind-body connection through her work for various health and wellness platforms. She is also a licensed massage therapist who has contributed meditations, essays, and blog posts to apps and websites focused on mental health and fitness.

Dr. Mala, is the Chief Clinical Officer at Recovery.com, where she develops impartial and informative resources for people seeking addiction and mental health treatment.




Hannah is a holistic wellness writer who explores post-traumatic growth and the mind-body connection through her work for various health and wellness platforms. She is also a licensed massage therapist who has contributed meditations, essays, and blog posts to apps and websites focused on mental health and fitness.

Dr. Mala, is the Chief Clinical Officer at Recovery.com, where she develops impartial and informative resources for people seeking addiction and mental health treatment.
When a doctor prescribes pain medication, we generally trust that it’s safe. Plenty of people take prescription painkillers like tramadol as directed and never have problems. But for some, what started as legitimate pain management becomes something much more concerning.
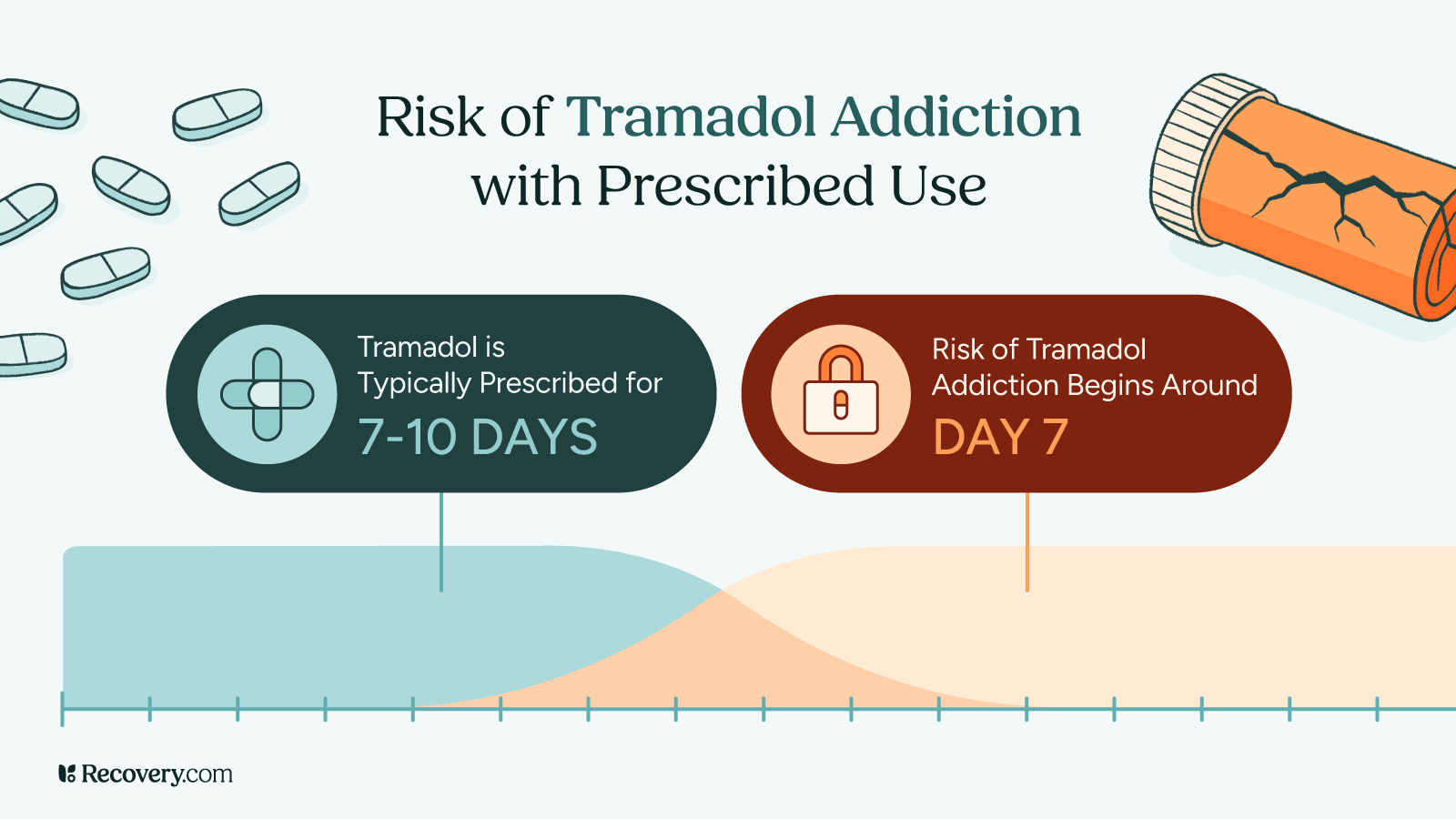
The reality is that tramadol addiction can develop even when you follow your doctor’s instructions. If you feel like your relationship with tramadol has gotten out of control, it’s because you’re dealing with a habit-forming substance that affects your brain chemistry.
We’ll explain how tramadol addiction develops and how to recognize the warning signs, understand the health risks, and explore proven treatment options.
What Is Tramadol?
Tramadol is a prescription opioid pain medication doctors commonly prescribe for moderate to severe pain. You might know it by brand names like Ultram, ConZip, or Ryzolt. Tramadol was initially thought to have a lower risk for addiction, which is why some doctors preferred it over stronger opioids like oxycodone or morphine.1
This medication works in the brain in 2 ways:
- First, it binds to opioid receptors like other painkillers.
- Second, it increases levels of serotonin and norepinephrine, brain chemicals that affect mood and pain perception.
This dual action makes tramadol effective for pain relief, but is also part of what makes it so likely to cause dependence.
Doctors often prescribe tramadol for conditions like arthritis, fibromyalgia, back pain, or recovery from surgery. Because it was considered “safer” than other opioids, many healthcare providers and patients alike initially viewed it as a lower-risk option. But research has shown that tramadol can indeed lead to physical dependence and addiction, even when you take it exactly as prescribed.2
The medication comes in immediate-release tablets (taken every 4-6 hours) and extended-release formulations (taken once or twice daily). Both forms can be addictive, though extended-release versions may create more consistent blood levels that can cause physical dependence over time.3

Can You Get Addicted to Tramadol?
Yes, you can develop tramadol addiction even when following your doctor’s orders. This may come as a surprise, since tramadol was marketed as having lower addiction potential. Studies show tramadol dependence affects up to 2–19% of those who take it, with most research finding rates above 5% in higher-risk groups.4
There’s an important difference between physical dependence and addiction. Physical dependence means your body has adapted to the medication and needs it to function normally and you’ll experience withdrawal symptoms if you stop suddenly. This can happen to anyone taking tramadol regularly for several weeks.
Addiction is a behavioral and psychological condition wherein you’re unable to stop using, even though you may want to. You might think about tramadol frequently, take more than you’re prescribed, or keep using it even when it’s causing problems. Addiction changes how your brain responds to rewards and stress.
Several factors increase addiction risk:5
- Personal or family history of substance use disorders
- Mental health conditions like depression or anxiety
- Past trauma
- Age (younger adults have higher addiction rates)
While risk factors might increase the likelihood of someone becoming addicted, addiction can affect anyone.
Physical dependence can begin within just days to weeks of regular use.6 Some people notice they need tramadol just to feel normal, while others realize they’re taking it for reasons beyond pain relief. If you’re concerned about your use, pay attention to your instincts.
1. Physical Changes
- Your usual dose doesn’t work as well anymore, so you need more
- You feel sick when you miss a dose (nausea, sweating, anxiety, like you have the flu)
- You can’t get through the day without taking tramadol
- You keep taking it even though your pain is better
2. Changes in How You Think and Act
- You think about tramadol a lot throughout the day
- You plan your schedule around when you can take your next dose
- You take more pills than your doctor prescribed
- Your prescription runs out before it should
- You visit different doctors to get more prescriptions
3. Emotional Changes
- You feel anxious or down when you haven’t taken tramadol recently
- Your mood depends on when you last took a dose
- You reach for tramadol when you’re stressed, not just when you’re in pain
- You get upset when family or friends ask about your medication use
- You find yourself making excuses for why you took extra pills
4. Effects on Daily Life
- Your tramadol use is causing problems with family, friends, or at work
- You’ve stopped doing things you used to love doing
- You’re not keeping up with important responsibilities
- Even though it’s causing problems, you can’t seem to stop
Once you understand the warning signs, it’s also important to know how tramadol affects your body both now and over time.
Tramadol’s Side Effects and Long-Term Health Impacts
Tramadol can affect your body in different ways, whether you’ve just started taking it or have been using it for a while. Right away, you might notice nausea, dizziness, feeling sleepy, or getting constipated. Many people also get dry mouth, headaches, and fatigue.
Mental Health
Your mental health can change with long-term use. At first, tramadol might actually make you feel better emotionally, but over time it can lead to depression and anxiety.7 You might find it harder to concentrate, have trouble remembering things, or feel emotionally disconnected.
Seizure Risk
One serious risk that’s unique to tramadol is seizures.8 This can happen even if you’ve never had a seizure before. The risk goes up if you take more than you’re supposed to or mix tramadol with other drugs or alcohol. This risk doesn’t go away even if you’ve been taking it for a long time.
Long-Term Physical Consequences
If you use tramadol for months or years, it can damage your liver, especially if your pills also contain acetaminophen (like Ultracet).9 It can also affect your respiratory system as well as your hormones, which might impact your ability to have children, your sex life, and your bone strength.
It can also affect your cardiovascular system, causing changes in heart rate and blood pressure. And opioid medications affect your body’s natural pain response, which might make you more sensitive to pain over time.10
Why It’s Not Safe to Stop Tramadol Suddenly
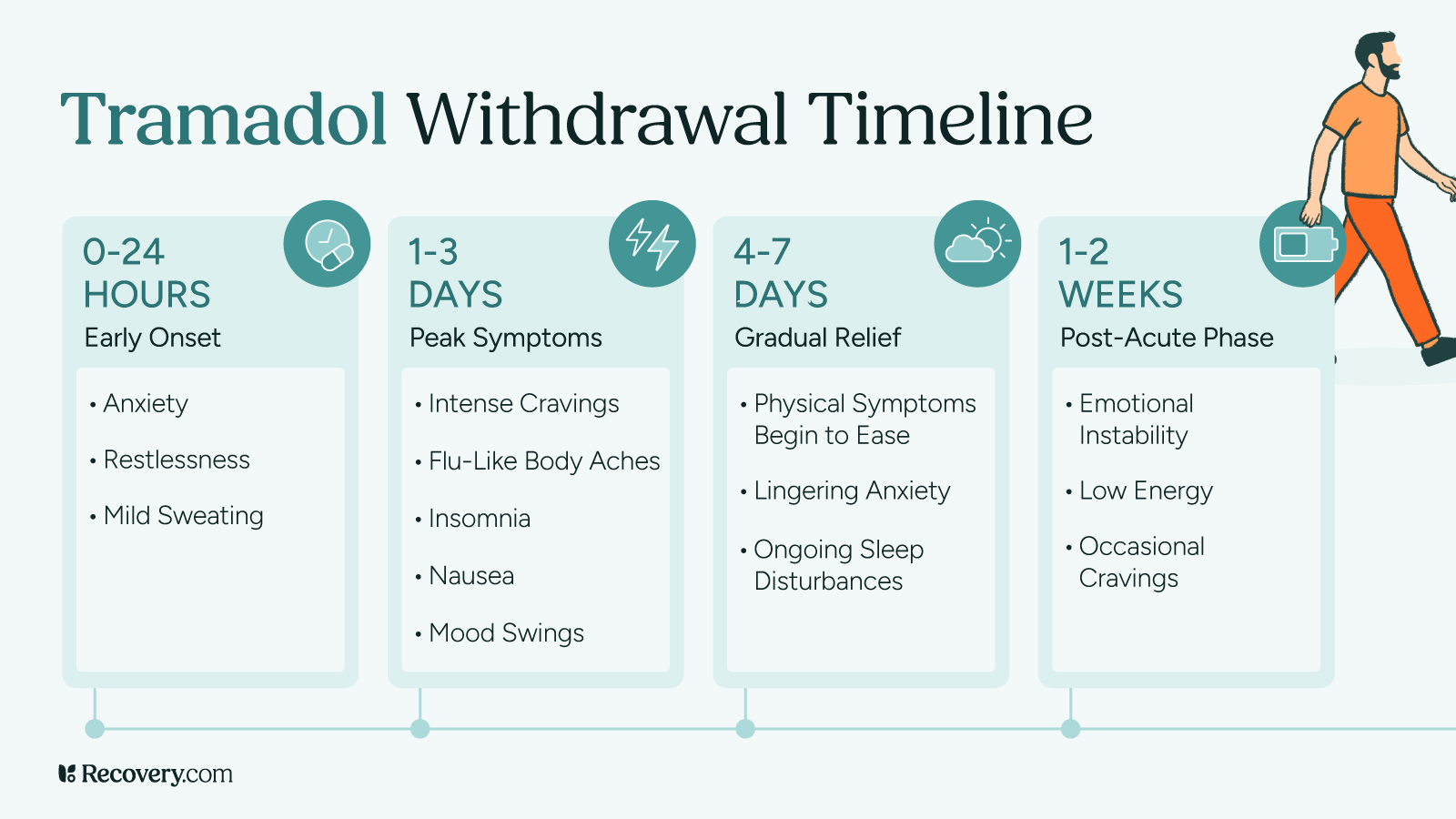
Stopping tramadol abruptly after regular use can be dangerous. Tramadol withdrawal is more complex than other opioid withdrawals, due to its unique effects on your brain chemistry.11
Common opioid withdrawal symptoms include nausea, vomiting, diarrhea, muscle aches, and flu-like symptoms. However, tramadol withdrawal often includes:
- Severe anxiety
- Panic attacks
- Confusion
- Hallucinations
- In some cases, seizures
Withdrawal typically begins 12–24 hours after your last dose, peaks around days 3–5, and acute symptoms can last 1–2 weeks. Some people have lingering depression, anxiety, and sleep problems for weeks or months after quitting.
Attempting to stop cold turkey often leads to relapse as the intense discomfort drives people back to using tramadol just to feel normal. That’s why it’s much better to work with a doctor who can help you slowly reduce your dose over time and give you medications to make the process more manageable.
Treatment Options for Tramadol Addiction
Getting your life back from tramadol addiction is absolutely possible with the right treatment approach. The most effective programs tackle the key areas: helping your body heal from physical dependence, addressing the psychological patterns that drive addiction, and rebuilding the relationships and life skills that addiction may have damaged.
Medical Detoxification
Medical detox is where you get professional help to safely stop using tramadol. A medical team monitors your vital signs, manages withdrawal symptoms as they come up, and steps in quickly if any complications develop. Most people complete this process in about 5–10 days.
The medical staff has tools to make you more comfortable during withdrawal—things like anti-nausea medications, sleep aids, and medications to reduce anxiety. They might also use medication-assisted treatment (MAT), where medications like buprenorphine actually reduce your cravings and withdrawal symptoms while blocking tramadol’s effects on your brain.
Learn more about what to expect during medical detox and how it can make the process safer and more comfortable in our detox FAQs.
Addiction Treatment Programs
Addiction treatment programs are designed to give you the tools and support you need for long-term recovery. These programs can happen in 2 main settings: residential (where you live at the treatment facility) or outpatient (where you attend sessions while living at home).
Most rehab programs combine several different approaches because what works varies from person to person. You’ll usually have individual therapy sessions where a therapist works with you one-on-one to create a treatment plan that fits your specific situation and needs. Group therapy is another core component—it connects you with others in recovery and provides a space to share experiences and learn from each other.
Many programs also use complementary therapies like art therapy, mindfulness training, or recreational activities to help you discover new ways to manage stress and find meaning. Support groups, both during treatment and as part of your ongoing plan, offer accountability and connection to sober community.
In rehab, your care team will customize your treatment plan based on your needs and what approaches seem to work best for you. There’s no one formula for recovery, which is why quality programs take the time to understand your individual situation and adjust your care as you progress.
Ongoing Recovery Support
Recovery doesn’t end when you complete a treatment program—it’s really just the beginning. After treatment, it’s a good idea to keep meeting regularly with your therapist to work through challenges and strengthen the coping skills you learned.
It’s important to lean into your support network during this phase. This might mean repairing relationships with family and friends who support your journey—and getting honest about relationships that don’t. Creating new connections that are centered on sober activities is a great way to maintain your sobriety and have a more meaningful, fun experience in recovery.
How Medications for Opioid Use Disorder Work
Medication-assisted treatment (MAT) uses prescription medications that work on the same parts of your brain as tramadol, but in a safer way that’s controlled by your medical team. When used correctly, they can reduce cravings and withdrawal symptoms, giving you space to focus on recovery. This therapy uses opioid replacement medications like buprenorphine and methadone or opioid blockers like naltrexone.
Some people worry that using these medications is just trading one addiction for another, but the reality is more nuanced than that. These are proven medical treatments that can help your brain heal while you learn long-term coping skills in therapy. It isn’t for everyone, but research shows that MAT can improve recovery outcomes and reduce the risk of overdose.12
Finding Help and Support
If you’re struggling with tramadol addiction, there’s good news: Addiction is very treatable.
Recovery.com can help you find effective treatment for opioid addiction. Search for a treatment program that matches your needs, and take the first steps toward a healthier, tramadol-free life.
FAQs
-
Ojha, R., & Bhatia, S. C. (2010). Tramadol dependence in a patient with no previous substance history. Primary care companion to the Journal of clinical psychiatry, 12(1), PCC.09100779. https://doi.org/10.4088/PCC.09100779ecr
-
Lanier, R. K., Lofwall, M. R., Mintzer, M. Z., Bigelow, G. E., & Strain, E. C. (2010). Physical dependence potential of daily tramadol dosing in humans. Psychopharmacology, 211(4), 457–466. https://doi.org/10.1007/s00213-010-1903-y
-
Lanier, R. K., Lofwall, M. R., Mintzer, M. Z., Bigelow, G. E., & Strain, E. C. (2010). Physical dependence potential of daily tramadol dosing in humans. Psychopharmacology, 211(4), 457–466. https://doi.org/10.1007/s00213-010-1919-3
-
Legasse, A. S., Tamiru, W., Mohammed, F., & Ataro, G. (2025). The prevalence of Tramadol abuse and associated factors among Hawassa University students, Hawassa, Ethiopia. PloS one, 20(3), e0318634. https://doi.org/10.1371/journal.pone.0318634
-
Danso, M., & Anto, F. (2021). Factors Associated with Tramadol Abuse: A Cross-Sectional Study Among Commercial Drivers and Assistants in the Accra Metropolitan Area of Ghana. Drugs - real world outcomes, 8(3), 337–347. https://doi.org/10.1007/s40801-021-00247-6
-
Lanier, R. K., Lofwall, M. R., Mintzer, M. Z., Bigelow, G. E., & Strain, E. C. (2010). Physical dependence potential of daily tramadol dosing in humans. Psychopharmacology, 211(4), 457–466. https://doi.org/10.1007/s00213-010-1919-3
-
Rougemont-Bücking, A., Gamma, F., & Panksepp, J. (2017). Use of tramadol in psychiatric care: A comprehensive review and report of two cases. Swiss Medical Weekly, 147, w14428. https://doi.org/10.4414/smw.2017.14428
-
Jick, H., Derby, L. E., Vasilakis, C., & Fife, D. (1998). The risk of seizures associated with tramadol. Pharmacotherapy: The Journal of Human Pharmacology and Drug Therapy, 18(3), 607–611. https://doi.org/10.1002/j.1875-9114.1998.tb03123.x
-
Hafez, E. (2022). Parenchymatous toxicity of tramadol: Histopathological and biochemical study. Journal of Alcoholism & Drug Dependence, 10(1), 1–6. https://doi.org/10.4172/2329-6488.1000225
-
Joseph, E. K., Reichling, D. B., & Levine, J. D. (2010). Shared mechanisms for opioid tolerance and a transition to chronic pain. The Journal of neuroscience : the official journal of the Society for Neuroscience, 30(13), 4660–4666. https://doi.org/10.1523/JNEUROSCI.5530-09.2010
-
Rajabizadeh, G., Kheradmand, A., & Nasirian, M. (2009). Psychosis following Tramadol Withdrawal. Addiction & health, 1(1), 58–61.
-
McKay, C. D., & CAADC (2017). Medication Assisted Treatment for Opioid Use Disorder. Delaware journal of public health, 3(4), 46–49. https://doi.org/10.32481/djph.2017.08.011
Our Promise
How Is Recovery.com Different?
We believe everyone deserves access to accurate, unbiased information about mental health and recovery. That’s why we have a comprehensive set of treatment providers and don't charge for inclusion. Any center that meets our criteria can list for free. We do not and have never accepted fees for referring someone to a particular center. Providers who advertise with us must be verified by our Research Team and we clearly mark their status as advertisers.
Our goal is to help you choose the best path for your recovery. That begins with information you can trust.










