Kratom Addiction and Withdrawal: Signs, Symptoms, and How to Get Help



Stacy Mosel is a licensed social worker, psychotherapist, and substance abuse specialist. After receiving a Bachelor's degree in Music from the State University of New York at Stony Brook, she continued her studies at New York University, earning a Master's of Social Work degree in 2002.

Kristen Fuller, M.D., enjoys writing about evidence-based topics in the cutting-edge world of mental health and addiction medicine and contributes to medicine board education.




Stacy Mosel is a licensed social worker, psychotherapist, and substance abuse specialist. After receiving a Bachelor's degree in Music from the State University of New York at Stony Brook, she continued her studies at New York University, earning a Master's of Social Work degree in 2002.

Kristen Fuller, M.D., enjoys writing about evidence-based topics in the cutting-edge world of mental health and addiction medicine and contributes to medicine board education.
Kratom is a naturally occurring herbal substance that produces effects similar to those of stimulants (amphetamines, cocaine) and opioids (heroin, morphine).1
While there isn’t enough evidence to confirm that kratom is addictive and can result in a substance use disorder (SUD), misusing kratom can lead to physical dependence and potentially dangerous health effects.1
Kratom use can be risky because the effects are largely unknown. Kratom may contain unlisted additives and can have mild to severe adverse consequences.1 As a result, the United States and international agencies have concerns about kratom.1
If you use kratom, or you know someone who does, this article will help you understand what kratom is, its effects, signs of misuse, and how to seek help if you’re struggling with kratom misuse or opioid use disorder.
What Is Kratom?
Kratom is a substance made from the leaves of a tropical tree known as Mitragyna speciosa that is native to Southeast Asia.1,2 Its leaves can be chewed or dried to be swallowed or brewed into teas and are often labeled as “herbal supplements” and sold over the counter.1,2
Kratom is a popular substance because it can produce euphoric effects similar to stimulants and the pain-relieving effects of opioids. Kratom is believed to act on the mu-opioid receptors in the brain, producing partial opioid-like effects at high doses.
When taken at low doses, kratom can produce similar effects to stimulants, which include increased alertness and energy, and a heightened sense of arousal and happiness.1,2 The medicinal use of kratom in Southeast Asia has a long history, dating back hundreds of years.3
Widespread kratom use in the U.S. is relatively new.3 However, in recent years, medical professionals, the U.S. Drug Enforcement Agency (DEA), U.S. Department of Agriculture (USDA), and the U.S. Food and Drug Administration (FDA) have shown concerns about kratom use.1
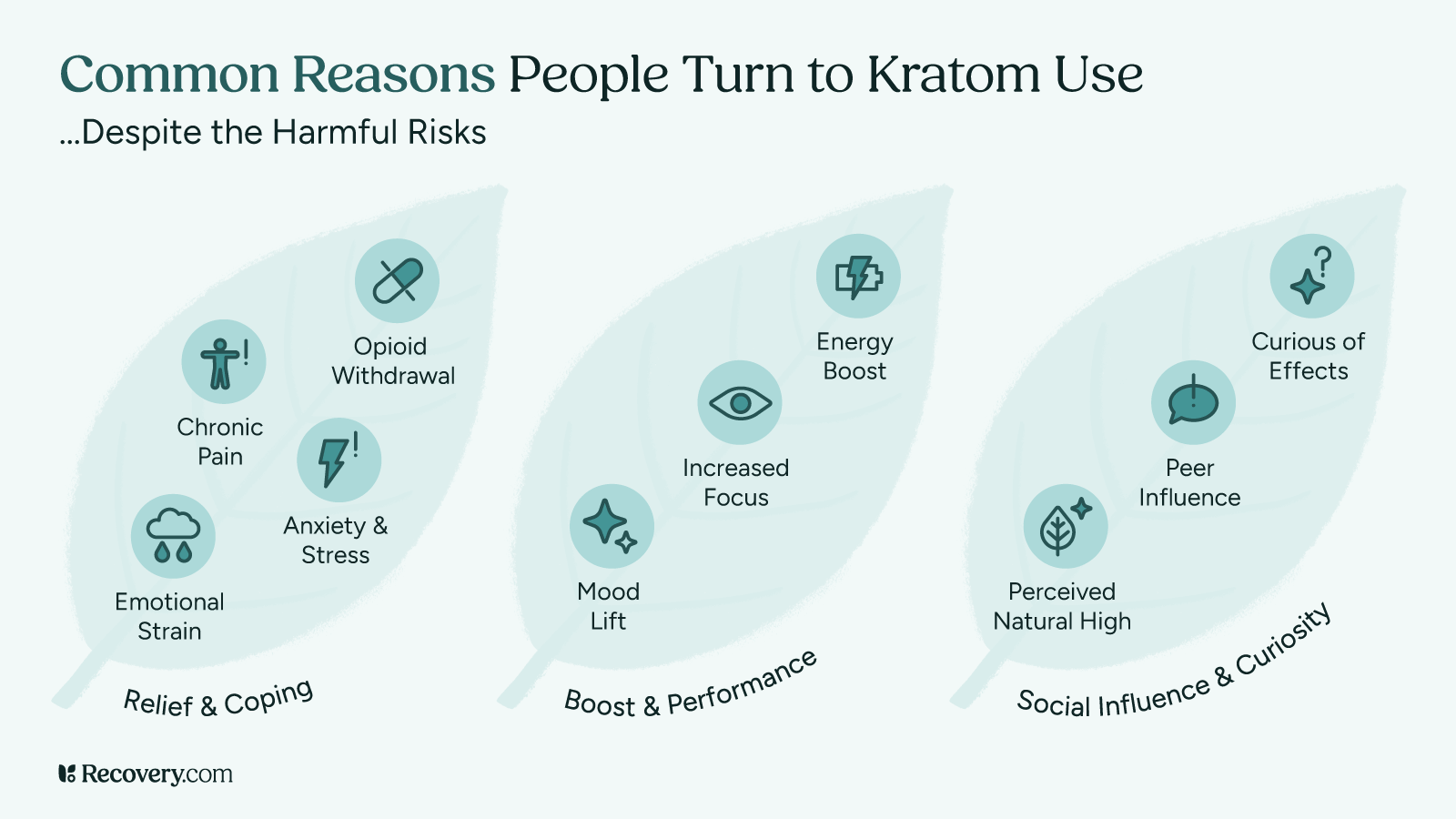
What Is Kratom Used For?
Kratom is often used to help alleviate chronic pain and opioid withdrawal symptoms because many people think it’s safer than opioids. However, more extensive research still needs to be done to prove this.1
People sometimes misuse kratom for its euphoric, relaxing, and stimulating effects. Kratom is often marketed as an appetite suppressant and a remedy for anxiety, depression, and panic attacks.1,3
Kratom use has increased in popularity in Western countries over the past decade; current estimates are that as many as 5 million individuals in the U.S. use kratom regularly.3
Is Kratom Legal in the U.S.?
Kratom is still legal in the U.S., though some countries have banned kratom products.1 The DEA has classified kratom as a “drug and chemical of concern,” but it is not listed as a controlled substance under the Controlled Substances Act.2,3 Regulations about kratom possession and use may differ by each state.2,3
The DEA proposed assigning kratom as a Schedule 1 controlled substance (the same category as heroin), resulting in the possession of kratom being illegal.3 However, this decision was put on hold due to severe backlash from many consumers in the U.S. who state that kratom has beneficial properties in treating opioid dependence and withdrawal symptoms.3
Kratom and associated products are still considered legal substances and available in many areas, though authorities like the FDA conduct ongoing reviews that help to inform policies regarding kratom.1 The FDA has advised consumers that they should not use kratom products due to the potential for adverse effects.1
What Are Kratom’s Effects?
While kratom is not yet fully understood, scientists know that it produces its effects because it contains many different chemical compounds.1
As with any substance, kratom's effects can vary based on several factors, such as how much kratom a person takes, how they take it, if they use it with other substances, and whether they have co-occurring medical or psychological conditions.1
Research is still ongoing about the short- and long-term effects of kratom, so it’s difficult to predict the effects a person might experience, especially since products and formulations can vary widely.1 Additionally, some products contain contaminants like bacteria such as salmonella, which can result in unwanted and unpredictable effects.1
Kratom can produce opioid and stimulant effects.1 Stimulant effects tend to occur at low doses, and kratom opioid effects (sedative effects) can occur at high doses.3
Some of the stimulant effects of kratom include:1,3
- Increased alertness and energy.
- Rapid heart rate.
- Talkativeness.
The opioid-like effects of kratom include:1,3
- Relaxation.
- Sedation.
- Pain relief.
- Confusion.
Kratom use is not without potential health risks. Some of the reported adverse effects of kratom include:1,3
- Nausea.
- Weight loss.
- Muscle pain.
- Constipation.
- Dizziness.
- Drowsiness.
- Confusion.
- Seizures.
- Slowed breathing.
- Liver problems.
- Psychotic symptoms include hallucinations and delusions.
There have been reported deaths associated with kratom use, but most of these have occurred because people used kratom with other substances or unknown contaminants in the product.1
Is Kratom Addictive?
In short, kratom might be addictive. In terms of addiction, medically known as a substance use disorder (SUD), there isn't enough evidence-based research to determine whether kratom is addictive.1
It’s believed that misuse may cause kratom dependence due to its stimulant and opioid-like painkilling effects.4
Dependence occurs over time when a drug is misused to the point that the body believes it needs it to function properly.
As a result of physical dependence, when the dosage is reduced or drug use stops completely, the individual may experience withdrawal symptoms.5 Research is ongoing to investigate kratom withdrawal and addictive potential.1,3,5
Dependence is not always associated with addiction meaning that an individual can be dependent on a substance but not addicted to kratom. The main concerns are the potentially dangerous effects of kratom misuse and the uncomfortable withdrawal symptoms.1
Can You Quit Kratom Cold Turkey?
Currently, there is no conclusive evidence on the extent of withdrawal symptoms caused by kratom use.1,3 While research is ongoing, studies suggest that kratom can lead to mild to moderate withdrawal symptoms when a person stops or reduces use.1,3
Quitting kratom “cold turkey” may be uncomfortable, but it does not appear to have any life-threatening side effects associated with its use or its withdrawal syndrome.
However, because so little is known about the substance, it’s a good idea to get guidance from your doctor or another medical professional. Medical detox can help ensure your comfort and safety and ease the transition to ongoing treatment, such as an inpatient or outpatient rehab program, which can help you maintain recovery.4
Stopping Kratom Use
Attempting to quit kratom on your own can be difficult. Many people use kratom to help alleviate chronic pain and opioid withdrawal symptoms, which can further complicate quitting.
If you’re trying to stop using kratom, you should know that professional help is available and can help manage the discomfort associated with withdrawal from kratom and opioid use disorder (OUD).1
- Seek professional help. Seek advice from your doctor or another medical professional. They can assess your health, provide referrals, and help create a personalized plan for stopping kratom safely that may involve detox and ongoing treatment programs.
- Actively participate in your program. Be willing to open up and address the root cause of your substance use. Therapy only works if a person makes an effort.
- Seek the support of loved ones. Knowing that at least one family member or friend loves and supports you can boost your motivation.
- Adopt healthy lifestyle changes. Incorporate regular exercise, a balanced diet, and sufficient sleep to support your physical and mental well-being.
- Set goals. Think about goals and aspirations that you may have had before using substances. Create measurable goals that you can work toward in the next six months, one year, and five years.
- Monitor and adjust. Regularly review your progress with your healthcare provider and adjust your plan as needed to address any challenges or setbacks.

Kratom Withdrawal: Timeline & Symptoms
Currently, there is no conclusive evidence on the withdrawal timeline of kratom. The onset of withdrawal and how long kratom withdrawal lasts may mimic that of opioid withdrawal, but more research is needed.5
Some studies suggest withdrawal symptoms may begin around 12 to 24 hours after a person last uses kratom and may last up to four days.6 Several factors can influence withdrawal, including how much kratom a person uses, for how long, and whether they use other substances.6
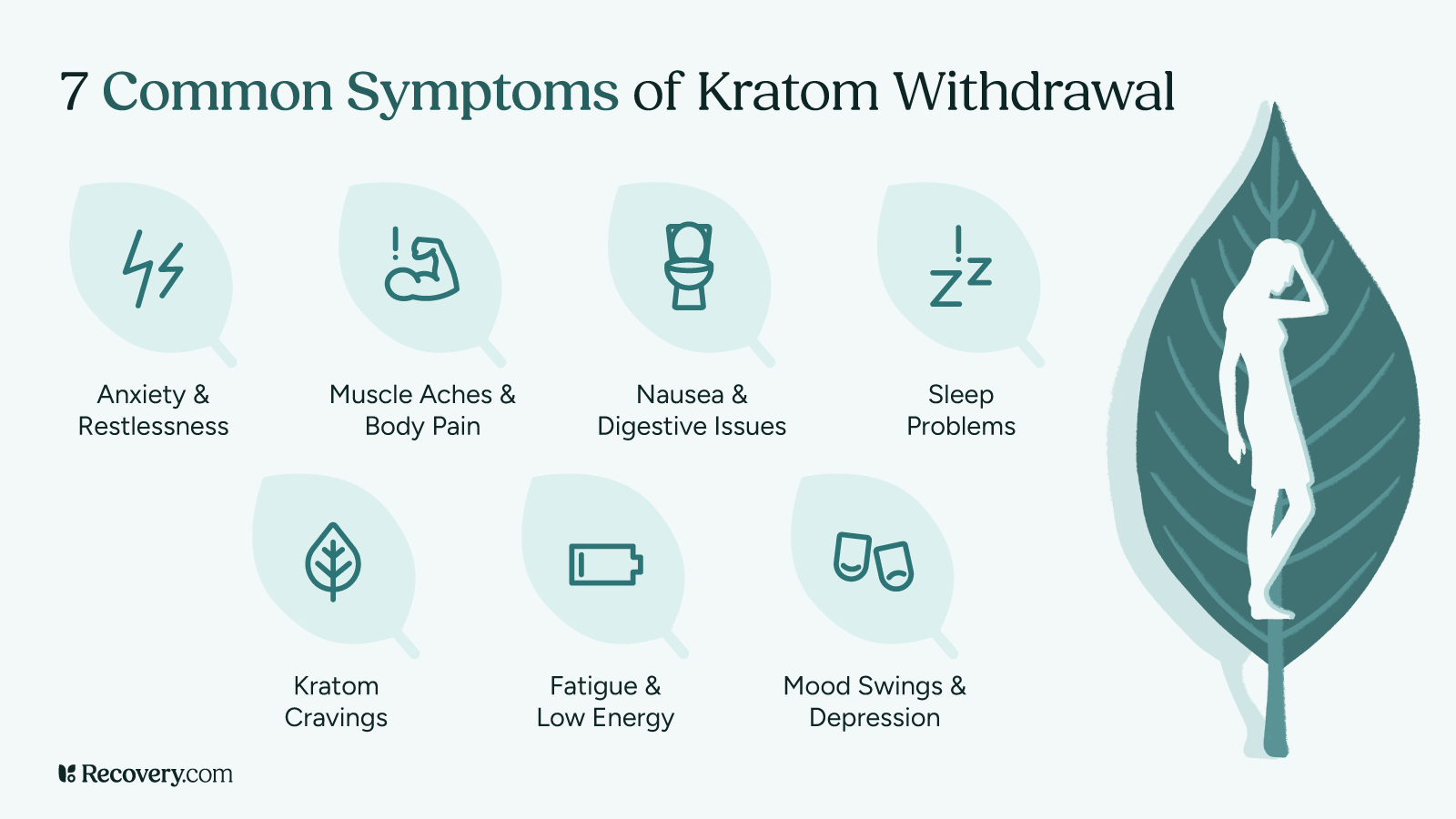
Kratom Withdrawal Symptoms
Kratom withdrawal symptoms may include:7
- Muscle aches.
- Insomnia.
- Aggression.
- Emotional changes.
- Runny nose.
- Jerky body movements.
Kratom Addiction Treatment: Rehab Options for Kratom
Although some people can quit taking kratom on their own, professional treatment provides several benefits to facilitate the process. Kratom addiction treatment centers and recovery programs include:8
- Medical detox: Medically managed kratom withdrawal in a detox center ensures that a person detoxes from kratom in a comfortable and safe environment. This can help patients more easily transition to ongoing treatment.
- Inpatient addiction treatment: Inpatient treatment programs involve living onsite full-time where a patient can focus on recovery. Programs vary but often include a combination of behavioral therapy, counseling, pharmacotherapy, and participation in support groups (e.g., 12-Step programs).
- Outpatient addiction treatment: Outpatient kratom recovery programs vary in duration, intensity, and setting. Examples of structured outpatient treatment approaches include partial hospitalization programs (PHP) and intensive outpatient programs (IOP). These programs often emphasize group therapy sessions, but provide individual and family therapy as needed.
- Rehab aftercare: Rehab aftercare can support a patient’s recovery after completing a formal treatment program. It can help patients maintain progress and prevent relapse. Aftercare activities include ongoing counseling and therapy, participation in support groups, residing in a sober living home, and more.
Ready to Start Your Recovery?
Kratom misuse can affect both health and quality of life, but recovery is possible with the right support. Use Recovery.com to find treatment programs near you that offer expert care, evidence-based therapies, and a path toward lasting healing.
FAQs
-
National Institute on Drug Abuse. (n.d.). Kratom. https://nida.nih.gov/research-topics/kratom
-
U.S. Drug Enforcement Administration. (April, 2020). Kratom.
-
Eastlack, S. C., Cornett, E. M., & Kaye, A. D. (2020). Kratom—Pharmacology, clinical implications, and outlook: a comprehensive review. Pain and therapy, 9(1), 55-69. https://pmc.ncbi.nlm.nih.gov/articles/PMC7203303/pdf/40122_2020_Article_151.pdf
-
Veltri, C., & Grundmann, O. (2019). Current perspectives on the impact of Kratom use. Substance abuse and rehabilitation, 10, 23–31. https://pmc.ncbi.nlm.nih.gov/articles/PMC6612999/pdf/sar-10-23.pdf
-
U.S. Drug Enforcement Administration. (2019, November). Kratom (Mitragyna speciosa korth). https://www.deadiversion.usdoj.gov/drug_chem_info/kratom.pdf
-
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing.
-
Stanciu, C. & Penders, T. (2020, October 6). Best practices in managing patients with Kratom addiction. https://pcssnow.org/wp-content/uploads/2020/09/KRATOM-webinar-PCSS-2020-final-version-9.28.20-1.pdf
-
National Institute on Drug Abuse. (2020, August 20). Commonly used drugs charts: Kratom. https://nida.nih.gov/research-topics/drugs-a-to-z#kratom
-
National Institute on Drug Abuse. (2017, May). How do medications to treat opioid use disorder work? . https://nida.nih.gov/research-topics/medications-opioid-use-disorder
Our Promise
How Is Recovery.com Different?
We believe everyone deserves access to accurate, unbiased information about mental health and recovery. That’s why we have a comprehensive set of treatment providers and don't charge for inclusion. Any center that meets our criteria can list for free. We do not and have never accepted fees for referring someone to a particular center. Providers who advertise with us must be verified by our Research Team and we clearly mark their status as advertisers.
Our goal is to help you choose the best path for your recovery. That begins with information you can trust.









