Rewiring Your Brain From Addiction: 7 Things You Need To Know



Hannah is a holistic wellness writer who explores post-traumatic growth and the mind-body connection through her work for various health and wellness platforms. She is also a licensed massage therapist who has contributed meditations, essays, and blog posts to apps and websites focused on mental health and fitness.

Dr. Mala, is the Chief Clinical Officer at Recovery.com, where she develops impartial and informative resources for people seeking addiction and mental health treatment.



Hannah is a holistic wellness writer who explores post-traumatic growth and the mind-body connection through her work for various health and wellness platforms. She is also a licensed massage therapist who has contributed meditations, essays, and blog posts to apps and websites focused on mental health and fitness.

Dr. Mala, is the Chief Clinical Officer at Recovery.com, where she develops impartial and informative resources for people seeking addiction and mental health treatment.
When you stop using drugs and alcohol, it takes time to rewire your brain. The exact timeframe depends on several factors. Certain drugs, for example, lengthen the brain rewiring process. Some practices can also help you recover faster.
Here’s what experts know about helping your brain rebuild after addiction:
1. Understanding How Addiction Changes Your Brain
Dopamine and the Brain’s Reward System
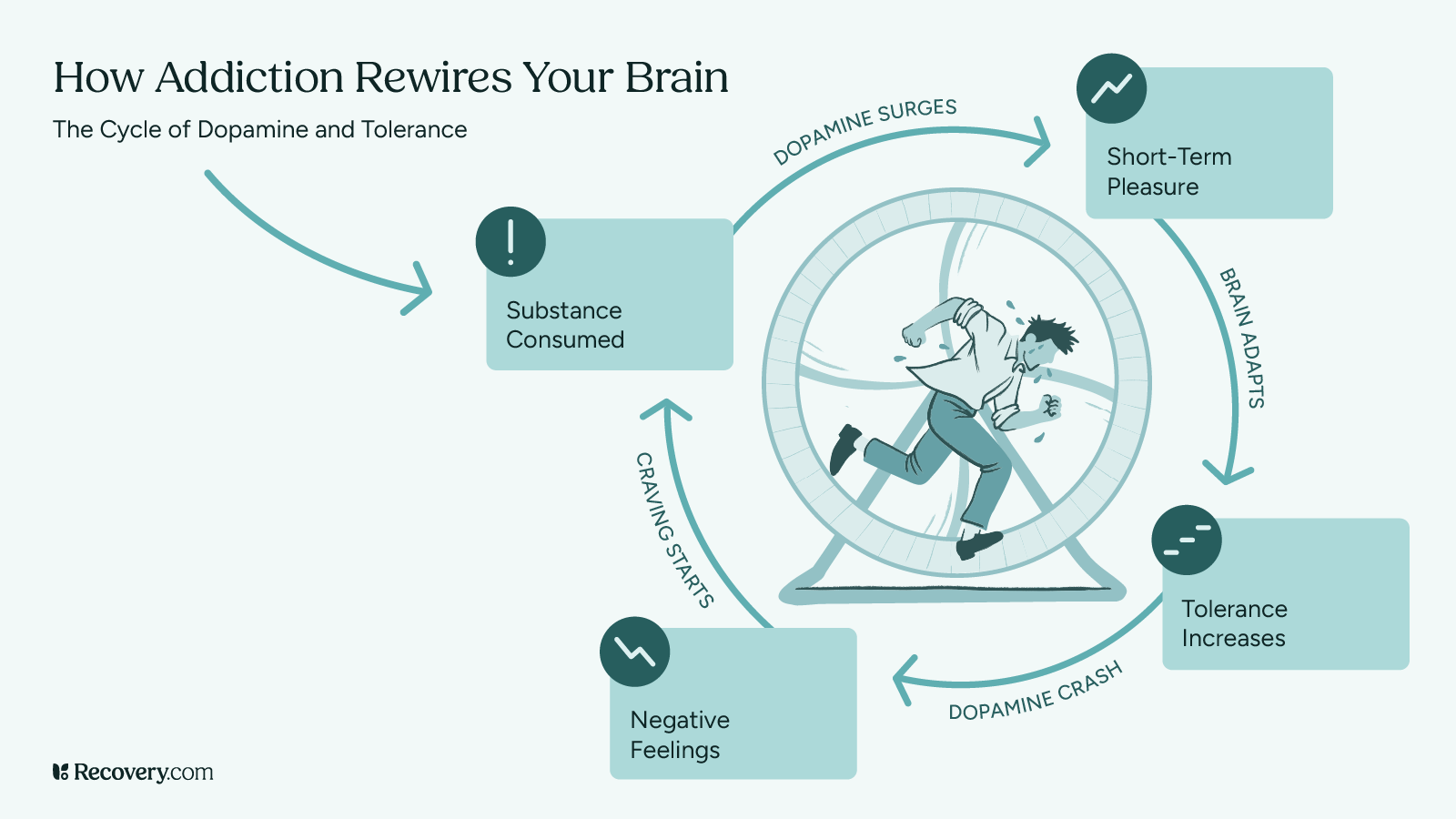
Your brain has a natural reward system that makes you feel good when you do things that help you survive and thrive.1 This system uses a neurotransmitter called dopamine, which creates feelings of pleasure and happiness. When you eat good food, exercise, or spend time with people you love, your brain releases small amounts of dopamine.
Alcohol and drug use release far more brain chemicals than natural activities do.2 This creates an unnaturally strong surge of pleasure signals in your brain. When this happens repeatedly, it can overwhelm your brain’s normal reward system.
Over time, your brain tries to adjust to these high levels of dopamine by becoming less sensitive to it. This means you need more and more of the substance to feel the same effects: a process we call tolerance.3 Regular stimuli that used to make you happy might not feel as good anymore, because your brain’s reward system isn’t working like it should.
Areas of the Brain Affected by Addiction
Addiction affects 3 main parts of your brain.4 Each plays a crucial role in helping you think, feel, and make decisions.
The basal ganglia is your brain’s pleasure center. It helps you feel good when you do healthy things like eating or exercising. With substance use disorders, this area becomes less sensitive to normal pleasures and more focused on substances.
The amygdala is your brain’s stress manager. When addiction develops, this area becomes more sensitive. This can make you feel anxious, irritable, or uncomfortable when you’re not using addictive substances.
The prefrontal cortex helps you make good decisions and control impulses.5 Addictive behaviors make this area weaker, which makes it harder to resist cravings or think about long-term consequences.

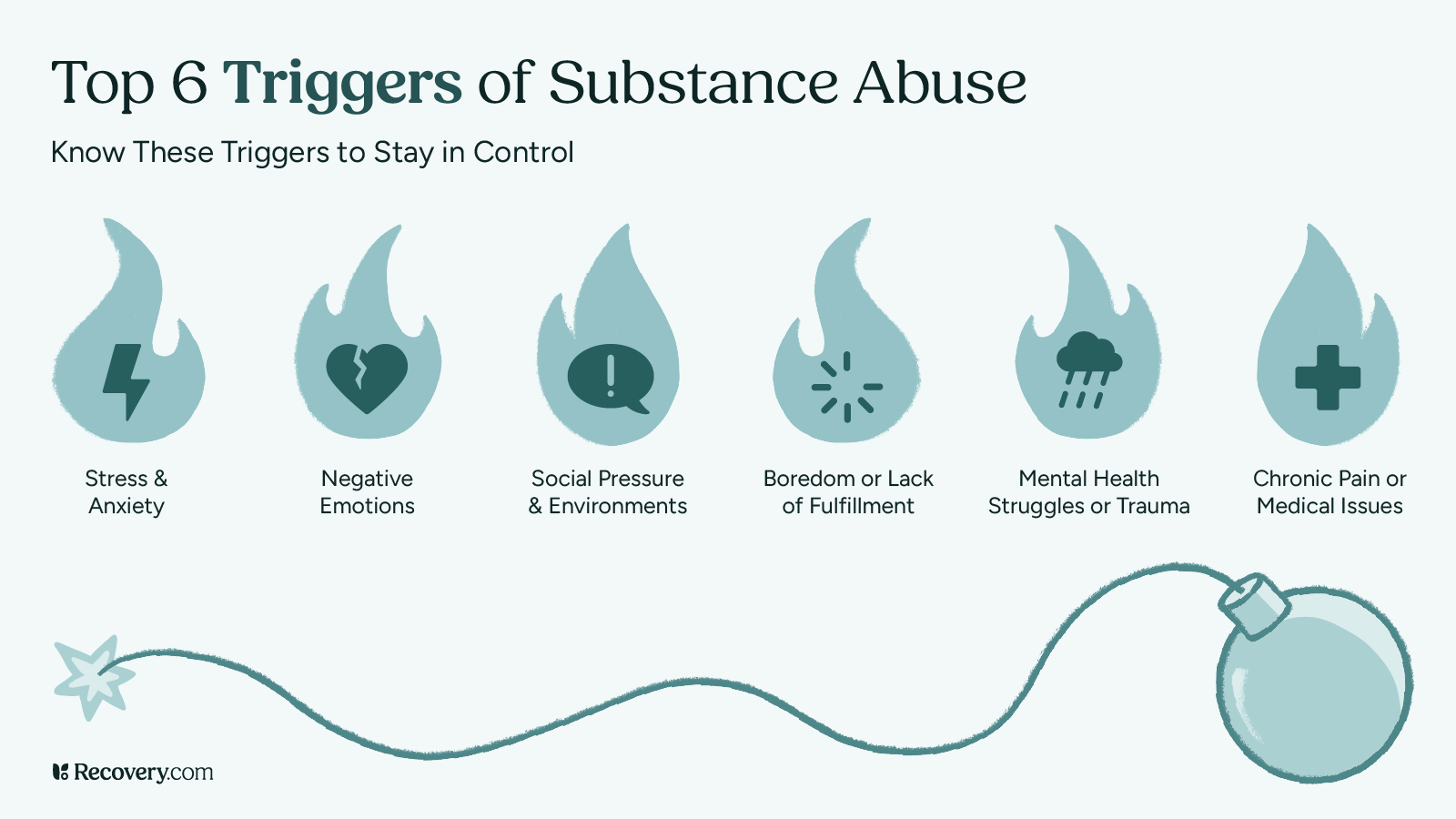
How Habits and Triggers Form
Your brain is designed to help you repeat behaviors that make you feel good. During addiction, your brain creates strong connections between certain situations (called triggers) and substance abuse. These connections form through repeated use over time.
Triggers can be places, people, feelings, or times of day that your brain associates with drug abuse. When you encounter these triggers, your brain automatically generates cravings. Learning to understand and manage your triggers (and their associated coping mechanisms) is an important part of recovery.
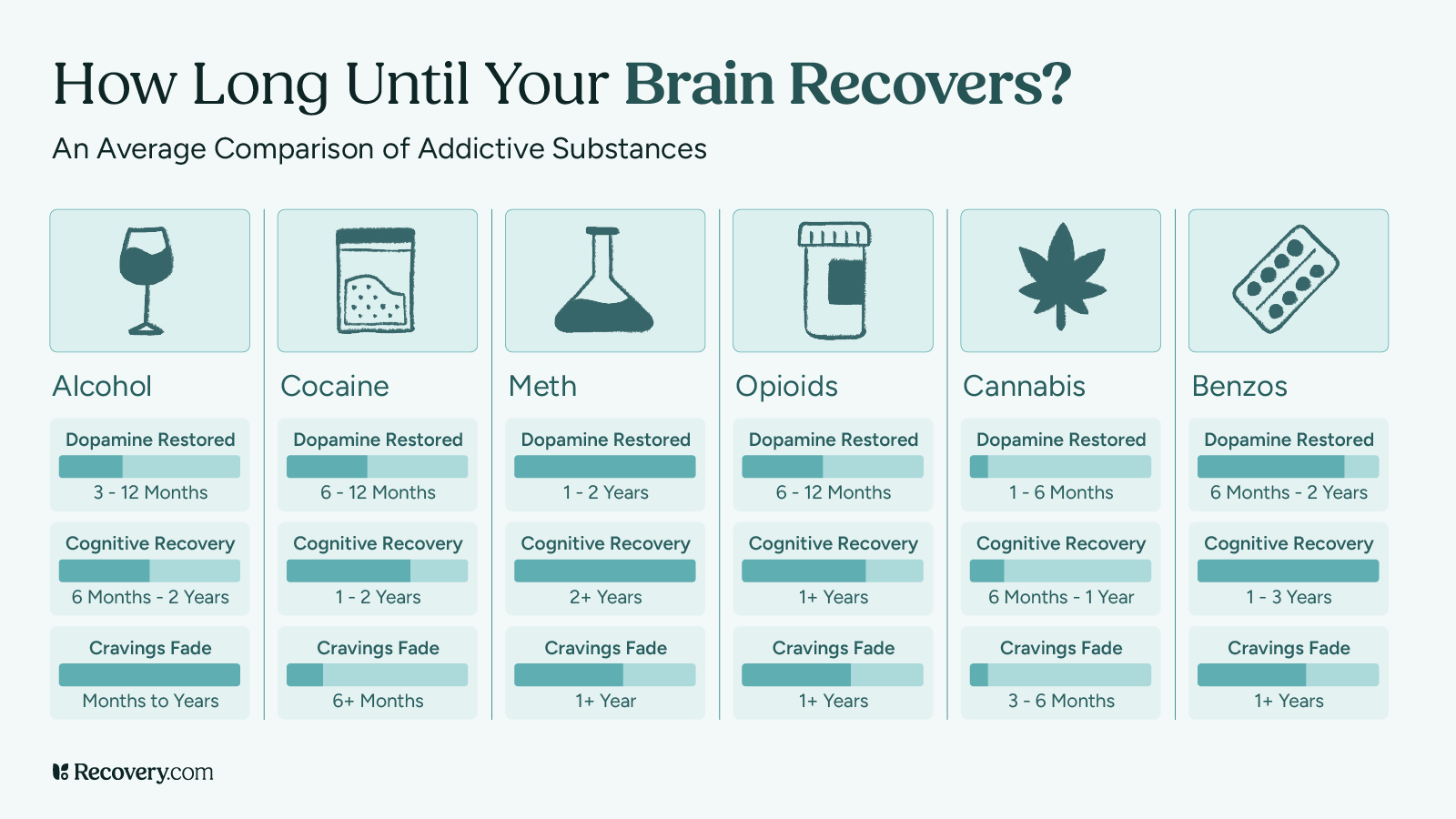
2. The Timeline of Brain Recovery
The recovery process happens in stages, and everyone’s path is different. While your brain health starts to improve as soon as you stop using substances, the full process takes time. Knowing what to expect during each stage can help you see the progress you’re making, which helps you stay motivated.
What to Expect in the First Month
The first month of recovery usually involves the biggest changes as your body adjusts to being substance-free. During the first week, you might experience withdrawal symptoms as your brain chemistry starts to reset. These symptoms can be uncomfortable, but they usually peak within a few days.
After the first week, many people notice their thinking becomes clearer and their sleep starts to improve. You might have mood swings or strong cravings during this time, which is normal. Your brain is working hard to restore its natural chemical balance.
Some people also notice changes in their appetite and energy levels during this first month. These changes are signs that your brain and body are beginning to heal.
Changes During Months 2-12
During these months, your brain continues to heal and rebuild healthy pathways. A lot of people in this stage find their mood becomes more stable and they start enjoying regular activities again. Your sleep quality and energy levels will continue to improve during this time.
Your brain’s ability to think clearly and make decisions also typically gets better during these months. But you might still experience occasional cravings—especially during stressful times. If this is the case for you, you’re not doing anything wrong! It’s totally normal and tends to happen less often as time goes on.
Your dopamine reward system will gradually become more responsive to natural pleasures like food, exercise, and social connections. This is a great sign that your brain is returning to its normal way of functioning.
Long-Term Recovery: One Year and Beyond
After a year, many people find their brain function has significantly improved. While some people still experience occasional cravings, these are usually less frequent and easier to manage. Your brain continues to heal and strengthen new, healthy patterns throughout your recovery journey.
Factors That Affect Your Recovery Timeline
Several things can influence how quickly your brain heals. These include the type of substances used, how long you used them, your overall health, and whether you have other mental health conditions. Having good support and treatment can help speed up the healing process.

3. Stages of Brain Rewiring
Just like healing from a physical injury, your brain goes through different stages as it recovers from drug addiction. While everyone’s journey is unique, knowing what to expect at each stage can help you feel more confident about the path ahead. Let’s look at how your brain heals over time.
Stage 1: Getting Through Withdrawal
The first stage of recovery starts when you stop using substances, and it’s often the most challenging part of the journey. During this time, your brain works hard to adjust to life without substances. You might feel physically and emotionally uncomfortable, which is completely normal.
Most people experience withdrawal symptoms for about a week, though this can vary depending on the substance. It’s very important to get medical support during this time, as some types of withdrawal can be dangerous. Remember, these difficult feelings are temporary and are signs that your brain is beginning to heal.
Stage 2: Early Recovery Changes
After withdrawal, you’ll enter a period where your brain is actively rebuilding healthy patterns. While you might still have cravings, they’ll likely feel less intense than before. This is the perfect time to start learning new ways to handle stress and challenging emotions.
During this stage, many people find it helpful to work with counselors or join support groups. These supports can teach you practical tools for managing cravings and building a healthy lifestyle. Your brain is becoming more receptive to new experiences and ways of coping.
Stage 3: Long-Term Healing
As you move into long-term recovery, your brain continues to strengthen its healthy pathways. While the journey doesn’t end here, many people find that cravings become less frequent and easier to handle. Each day of recovery helps your brain build and maintain these positive changes.
4. Supporting Your Brain’s Recovery
Fortunately, there are plenty of ways you can support your brain’s natural healing process. Think of recovery like tending a garden: The more care and attention you give it, the better it grows. Simple daily choices can make a big difference in how quickly and effectively your brain recovers.
Regular Exercise and Physical Activity
Moving your body is one of the best gifts you can give your healing brain. Exercise naturally boosts your mood by releasing feel-good chemicals, similar to the ones your brain is learning to produce again on its own. Even a 15-minute walk can help!6
You don’t need to live at the gym or start running marathons. Start with activities you enjoy, whether that’s dancing, swimming, or taking an easy walk around your neighborhood. As your energy improves, you’ll gradually be able to do more.
Sleep and Nutrition
Your brain does much of its repair work while you sleep, making good rest essential for recovery. Try to go to bed and wake up at the same time each day, even if you don’t feel tired at first. Your sleep patterns will naturally improve over time.
Eating nutritious foods gives your brain the building blocks it needs to heal. Instead of worrying about perfect eating habits, focus on adding healthy foods like fruits, vegetables, and proteins to your meals. Even small improvements in your diet can help your brain recover.
Stress Management
Finding healthy ways to handle stress is essential to your recovery journey. Deep breathing, taking short walks, listening to music, or talking with supportive friends all help calm your mind. Remember that it’s okay to start small—working in small moments of relaxation throughout your day can go a long way in calming your nervous system.
Building New Routines
Creating new daily routines helps your brain build healthy patterns. Start with one or 2 simple habits, like having breakfast at the same time every day or taking a walk after dinner. As these become comfortable, you can gradually add more supportive activities to your day.
5. Treatment Options That Help Rewire the Brain
Recovery isn’t a journey you need to take alone—there’s no shame in asking for help. Professional addiction treatment and support can have a huge impact on how quickly your brain heals. These interventions are like tools in your recovery toolkit: you can choose the ones that work best for you.
Therapy and Counseling
Working with a counselor or therapist gives you empowering tools for addiction recovery. These professionals understand how addiction affects the brain and can teach you practical ways to handle cravings and stress. Many people find cognitive behavioral therapy (CBT) especially helpful, as it teaches you how to change thought patterns that lead to substance abuse.7
Your therapist can act as a guide on your recovery journey, helping you understand your triggers and develop strategies that work for your specific situation. It’s a great idea to find a therapist you like and start building a relationship with them, so help is there when you need it.
Support Groups
Meeting others who understand what you’re going through can be incredibly motivating. Support groups are safe spaces to share your experiences, learn from others, and build connections with people who support your recovery goals.
Lifestyle Changes
Small changes in your daily life can support your brain’s healing process. Focus on one change at a time, like improving your sleep schedule or adding healthy activities you enjoy.
6. The Science of Hope and Healing
Understanding Brain Plasticity
Your brain has the ability to change and heal throughout your life. Scientists call this “plasticity,” which means your brain can create new neural pathways as it adapts to changes. This incredible ability is what makes recovery possible, no matter how long you’ve struggled with addiction.
Evidence of Recovery
Brain scanning studies show that people’s brains do heal during addiction recovery.8 While everyone’s timeline is different, many people see improvements in their cognitive functions, including memory, impulse control, decision-making, and emotional regulation. These positive changes only continue as you move forward in your recovery.
Setting Realistic Expectations
Recovery is more like a marathon than a sprint, and that’s okay. Some days will be easier than others, and healing happens gradually. Being patient with yourself and celebrating small victories along the way can help you stay on track.
7. Getting Help and Support
Finding Treatment
Taking the first step toward addiction treatment takes some courage, but the rewards of a life in recovery are well worth it. There are plenty of different treatment programs available to meet your specific needs, from detox to outpatient treatment to residential care. To learn more about choosing the right program, see our guide to finding a treatment center.
Building a Support System
Recovery is stronger when you have people in your corner. Loved ones, family, friends, counselors, support groups, and others in recovery can all be part of your support network. Don’t be afraid to let people know what you need.
If you’re ready to start recovery, a comprehensive rehab program can be a great starting point for your journey. This immersive experience gives you a chance to focus entirely on healing in a substance-free environment. Search for an addiction treatment center that matches your criteria and reach out to their team directly today.
FAQs
-
1. Volkow, N. D., Koob, G. F., & McLellan, A. T. (2016). Neurobiologic advances from the brain disease model of addiction. New England Journal of Medicine, 374(4), 363-371. https://doi.org/10.1056/NEJMra1511480
-
2. Nestler, E. J. (2013). Cellular basis of memory for addiction. Dialogues in Clinical Neuroscience, 15(4), 431-443. https://doi.org/10.31887/DCNS.2013.15.4/enestler
-
3. Koob, G. F., & Volkow, N. D. (2010). Neurocircuitry of addiction. Neuropsychopharmacology, 35(1), 217-238. https://doi.org/10.1038/npp.2009.110
-
4. Robinson, T. E., & Berridge, K. C. (2008). The incentive sensitization theory of addiction: Some current issues. Philosophical Transactions of the Royal Society B: Biological Sciences, 363(1507), 3137-3146. https://doi.org/10.1098/rstb.2008.0093
-
5. Goldstein, R. Z., & Volkow, N. D. (2011). Dysfunction of the prefrontal cortex in addiction: Neuroimaging findings and clinical implications. *Nature Reviews Neuroscience, 12(11), 652-669. https://doi.org/10.1038/nrn3119
-
6. Hyman, S. E., Malenka, R. C., & Nestler, E. J. (2006). Neural mechanisms of addiction: The role of reward-related learning and memory. *Annual Review of Neuroscience, 29*(1), 565-598. https://doi.org/10.1146/annurev.neuro.29.051605.113009
-
7. Kalivas, P. W., & Volkow, N. D. (2005). The neural basis of addiction: A pathology of motivation and choice. American Journal of Psychiatry, 162(8), 1403-1413. https://doi.org/10.1176/appi.ajp.162.8.1403
Our Promise
How Is Recovery.com Different?
We believe everyone deserves access to accurate, unbiased information about mental health and recovery. That’s why we have a comprehensive set of treatment providers and don't charge for inclusion. Any center that meets our criteria can list for free. We do not and have never accepted fees for referring someone to a particular center. Providers who advertise with us must be verified by our Research Team and we clearly mark their status as advertisers.
Our goal is to help you choose the best path for your recovery. That begins with information you can trust.









