How Long Does Psychosis Last? Navigating the 3 Stages From Onset to Recovery



Hannah is a holistic wellness writer who explores post-traumatic growth and the mind-body connection through her work for various health and wellness platforms. She is also a licensed massage therapist who has contributed meditations, essays, and blog posts to apps and websites focused on mental health and fitness.

Dr. Mala, is the Chief Clinical Officer at Recovery.com, where she develops impartial and informative resources for people seeking addiction and mental health treatment.



Hannah is a holistic wellness writer who explores post-traumatic growth and the mind-body connection through her work for various health and wellness platforms. She is also a licensed massage therapist who has contributed meditations, essays, and blog posts to apps and websites focused on mental health and fitness.

Dr. Mala, is the Chief Clinical Officer at Recovery.com, where she develops impartial and informative resources for people seeking addiction and mental health treatment.
When someone experiences psychosis, it changes how they understand the world around them. This can be scary and confusing, both for the person going through it and the people around them. Fortunately, psychosis can be treated, and many people regain stability and heal successfully with the right support.
We’ll explain what affects the duration of psychosis, how long related mental health issues typically last, and what recovery looks like. Whether you’re experiencing psychosis symptoms yourself, supporting someone who is, or just wanting to learn more, we’ll walk through what to expect in simple terms. Everyone’s experience with psychosis is different, but knowing the typical patterns can help you navigate this challenging time.
Let’s look at what psychosis is, how long it usually lasts, and what helps people heal.
What Is Psychosis?
Researchers define psychosis as “an amalgamation of psychological symptoms resulting in a loss of contact with reality.” About .5 to 3.5% of people are affected by psychotic disorders, and many more people experience a psychotic symptom of some kind at some point in their lives.1
The 3 Stages of Psychosis
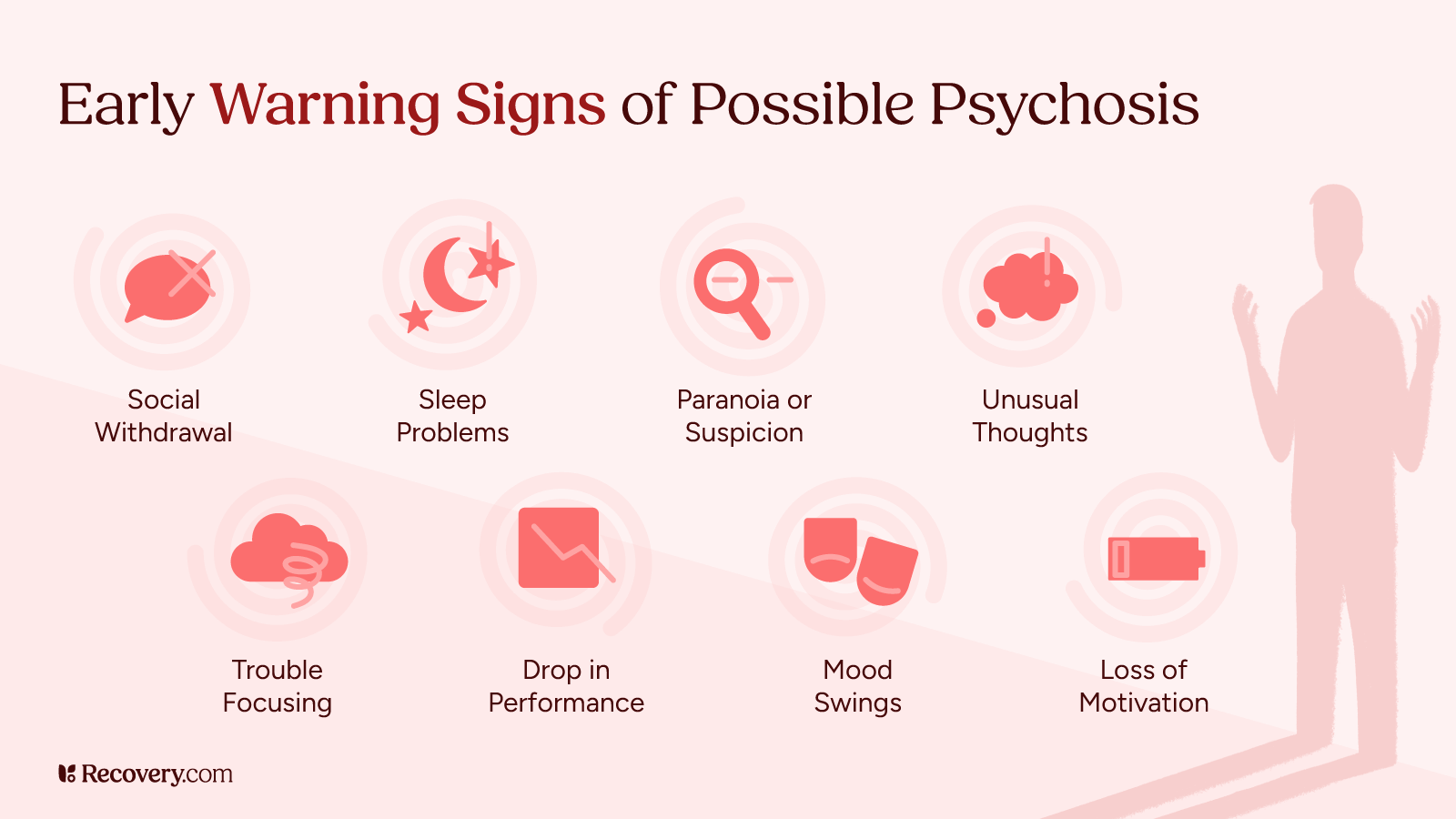
Understanding these stages of psychosis helps you recognize what’s happening and know what to expect:2
1. Prodromal Phase
The first stage is called the prodromal phase, also known as “psychosis syndrome.”3 You can think of it as the early warning period before full psychosis develops. During this time, you might notice subtle changes in thoughts and feelings. A person might start pulling away from friends and family, have trouble sleeping, feel suspicious of people around them, or suddenly struggle at work or school.
This early phase can last anywhere from a few days to several years. The tricky part is that many people don’t recognize these changes as warning signs of psychosis. They might just feel “off” or “not like themselves.” Family and friends are often the first to notice that something isn’t quite right.
2. Acute Phase
The acute phase is when psychosis becomes more obvious. This is when hallucinations (like hearing voices or seeing things that aren’t there) and delusions (strong, false beliefs) clearly appear. Someone might become convinced they’re being watched or persecuted, or they might talk about hearing voices that no one else can hear.
This phase typically lasts between a few days and several months. It’s usually the point when people finally get professional help because the symptoms are hard to ignore. Without treatment, this phase can last longer and symptoms may get worse.
3. Recovery Phase
The final stage—recovery—happens when people get adequate care. With appropriate treatment, symptoms gradually decrease. People begin to make sense of what happened and learn ways to manage their condition. They slowly get back to their regular activities and rebuild their relationships.
Recovery time varies a lot from person to person. Some people bounce back within weeks or months, while others might take a year or longer. As with any type of mental illness recovery, this process isn’t always linear—there are good days and tougher days along the way. But with the right treatment and support, most people see real improvement over time.
From your perspective, what are the most important factors that influence how long psychosis lasts—and why?

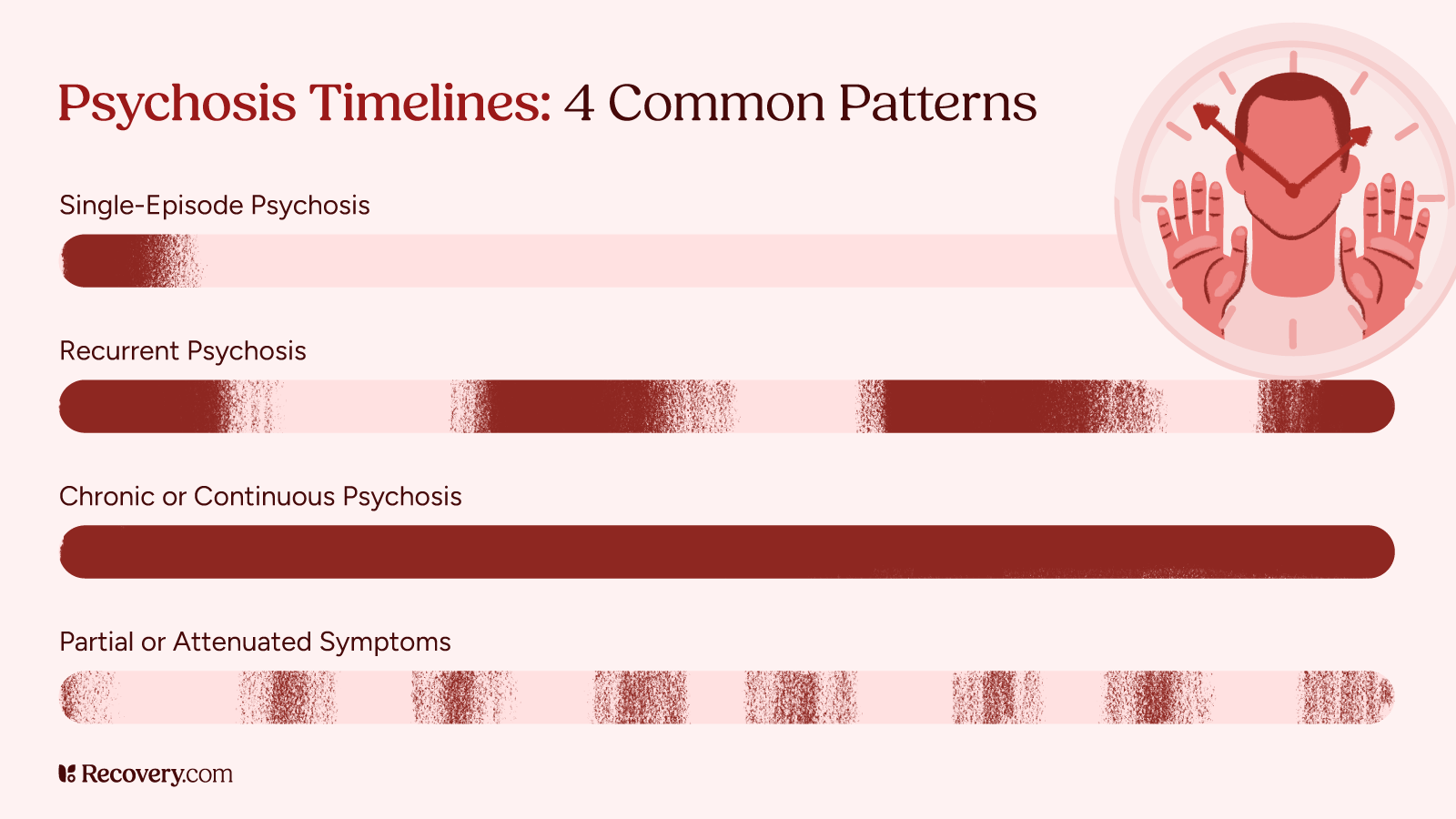
Duration of Different Types of Psychosis
Let’s talk about how long different types of psychosis typically last. Remember, each person’s experience is unique, but these timeframes can give you a general idea of what to expect.
Brief Psychotic Disorder
Sometimes psychosis appears suddenly after a major stress or trauma, like losing a loved one or experiencing a natural disaster. This is called brief psychotic disorder, and as the name suggests, it’s not permanent.4 Symptoms typically last between a day and a month, then go away completely. Most people who experience this type of psychosis make a full recovery without any long-term problems.
Drug-Induced Psychosis
Using certain drugs like marijuana, LSD, methamphetamine, or cocaine can trigger psychosis in some people. The good news is thatsubstance-induced psychosis usually clears up within a few days to a few weeks after the person stops using the substance (which may require professional addiction treatment). But for some folks—especially those who used drugs heavily or for a long time—symptoms might linger for months. In some cases, drug use can unmask an underlying mental health condition that requires ongoing treatment.
To learn more about how substance use can affect psychosis, see our article on thelink between addiction and schizophrenia.
Schizophrenia-Related Psychosis
When psychosis is part of schizophrenia, it follows a different pattern. People with schizophrenia often have episodes of psychosis that last between a few weeks and several months.5 Between these episodes, symptoms might decrease but rarely disappear completely without treatment. With proper medication and therapy, many people with schizophrenia can manage their symptoms well and reduce the frequency and intensity of psychotic episodes.
To learn more about comprehensive treatment options for schizophrenia and related psychosis, see our complete guide toschizophrenia rehab and recovery.
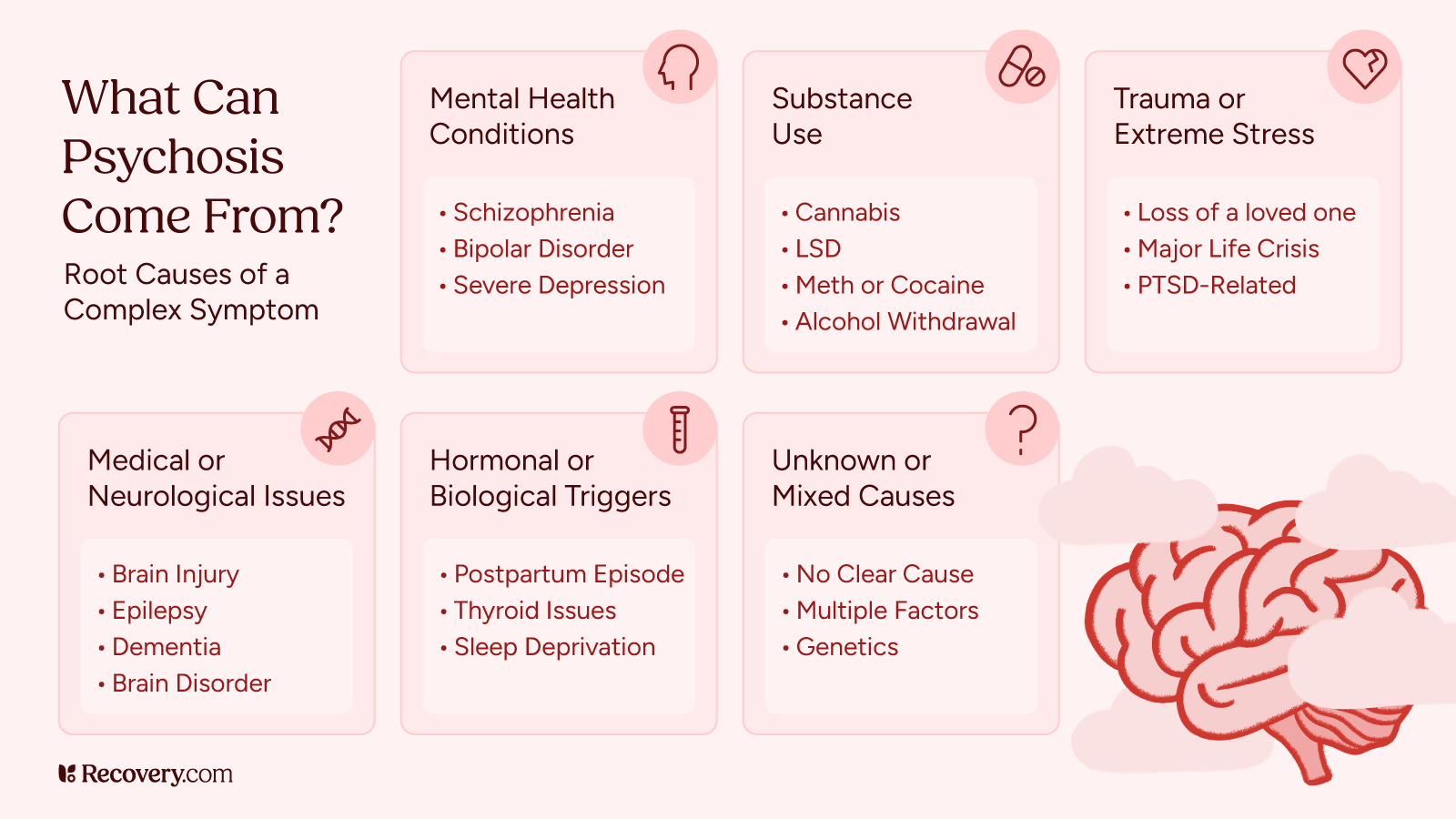
Mood Disorder Psychosis
Severe depression or bipolar disorder can sometimes include psychotic features.6 In bipolar disorder, psychosis usually appears during manic or depressive episodes and improves when the episode resolves. In a professional treatment program, the recovery process might take weeks to months. For depression with psychosis, symptoms often improve as the depression lifts, usually within a few months of starting treatment.
Postpartum Psychosis
Some new parents experience psychosis shortly after giving birth.7 This is a serious condition that usually develops within the first week after delivery. With quick treatment, postpartum psychosis typically improves within a few weeks to a few months. Most people recover completely, though they may have a higher risk of experiencing it again with future pregnancies.
Factors That Affect How Long Psychosis Lasts
Several factors can influence how long psychosis lasts and how well someone recovers. Understanding these can help you set realistic expectations about the recovery journey.
Early Intervention
One of the most important factors is how quickly someone gets help. The sooner someone starts treatment after their first episode, the better the outcomes tend to be. While research shows that it’s “common for a person to have psychotic symptoms for more than a year before receiving treatment,” says the National Institute of Mental Health (NIMH), “Reducing this duration of untreated psychosis is critical because early treatment often means better recovery.”8
Treatment Approach and Adherence
The type of treatment someone receives—and how well they stick with it—makes a huge difference. Most effective treatment plans include a combination of medication, therapy, and social support. Missing medication doses or stopping treatment too early can lead to longer episodes or relapses. It’s like treating any other health condition: Consistent, high-quality care leads to better results.
Treatment adherence is an ongoing issue in patients with psychosis—one study shows that over 60% of psychotic patients “had adherence difficulties at some point” in their program.9 That’s why behavioral health experts use interventions like family involvement, psychoeducation, and motivational interviewing to try to improve treatment outcomes.
Learn how therapists use specialized techniques to help you stay committed to your recovery journey in our guide tomotivational interviewing.
What’s something people often misunderstand about psychosis recovery that you wish more people knew?

Support System
Having supportive family, friends, and therapists can significantly shorten recovery time. People with strong support networks often recover faster because they have help navigating treatment, managing stress, and handling day-to-day responsibilities while they heal.10 If you’re supporting someone with psychosis, your patience and understanding matter more than you may realize.
Underlying Cause
The cause of psychosis affects its duration too. Psychosis triggered by stimuli like drug use or extreme stress often resolves more quickly than psychosis related to conditions like schizophrenia. Identifying and addressing the root cause is an important part of effective treatment.
Individual Factors
Every person is unique, and factors like previous psychotic episodes, stress levels, overall health, and even genetics can influence recovery time. As with physical illnesses, some people naturally recover more quickly than others.
Stress and Environment
High-stress environments can prolong recovery from psychosis or trigger relapses. Creating a calm environment that supports psychosis recovery can help shorten episodes and prevent them from recurring.11 Sometimes, simple changes at home, at work, or in social circles can make a big difference in someone’s recovery.
While these factors influence recovery time, they don’t determine it completely. Even when circumstances aren’t ideal, many people still recover well with the right treatment and support.
Treatment and Recovery
Getting the right treatment can make a huge difference in how long psychosis lasts and how well someone recovers. Let’s look at the most common treatments and what recovery looks like.
Psychiatry (Medication)
Antipsychotic medications are usually the first line of treatment for psychosis.12 These medicines help reduce hallucinations, delusions, and confused thinking, usually within a few days to a few weeks. Some people notice improvement very quickly; others might need to try different medications to find the right fit.
Most people take these medications for at least 6-12 months after an episode. Your doctor might recommend longer treatment depending on the underlying cause and whether you’ve had multiple episodes. Never stop taking medication suddenly—always work with your healthcare provider to make changes safely.
To learn more about how to work with your doctor to make sure your medication works for you, see our guide tomedication management.
Therapy Options
Medication works best when combined with therapy. When you access professional care, your treatment team can create a comprehensive treatment plan that combines medication, therapy, and other support. This might include psychotherapy like cognitive behavioral therapy (CBT), support groups, or social skills training, based on what best meets your needs.
Day-to-Day Support
Recovery isn’t just about medical treatment—it’s also about redesigning your daily life. This might include help with housing, employment, education, or building healthy routines. Some people work with case managers who can connect them with community resources and provide practical support during recovery.13
What to Expect During Recovery
Recovery from psychosis is usually gradual. Most people see significant improvement within a few months of starting treatment, though complete recovery can take longer. Schizophrenia survivor Sarah Ryan describesemotional recovery from psychosis as:
- Accepting a new normal: Accepting that while you may never be exactly the same person you were before psychosis, you can find pride in adapting to the new you
- Trusting yourself: Having patience and allowing positive experiences to accumulate over time, which gradually strengthens your confidence
- Believing in yourself: Choosing to value yourself despite a stigmatized diagnosis and maintaining hope that you can have a meaningful future
- Wanting to be yourself: Letting go of comparing yourself to “normal” people and recognizing that your life has value and purpose despite the challenges you’ve faced
Some people recover completely from psychosis. Others learn to manage occasional negative symptoms while leading full, meaningful lives. Many people worry about having another episode, which is a common concern. Working with your care team to identify early warning signs and create a relapse prevention plan can help you manage this fear as you keep taking steps forward.
How can family members or loved ones best support someone recovering from psychosis, especially in the early stages?

Finding Your Way Forward: Embracing Life After Psychosis
Recovery from mental health disorders is a challenging but rewarding process that involves ups and downs. But as Ryan says of her experience with psychosis recovery,14
For the first time, I can say with confidence that it is good and right to be me. My life is not a mistake, and good things have come out of my life that outweigh the bad. I can never truly make sense of what happened to me, but I have finally let go, because I have too many other great things to hold onto that are pulling me forward.
You, too, can come to see the great things that are pulling you forward—and professional care can help. If you’re experiencing symptoms of psychosis, don’t wait to get help.Reach out to a mental health professional today and give yourself the best chance of recovery.
FAQs
-
Calabrese J, Al Khalili Y. Psychosis. [Updated 2023 May 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK546579/
-
What Is Psychosis. https://medicine.yale.edu/psychiatry/step/psychosis/. Accessed 10 Apr. 2025.
-
Addington J. The prodromal stage of psychotic illness: observation, detection or intervention? J Psychiatry Neurosci. 2003 Mar;28(2):93-7. PMID: 12670126; PMCID: PMC161730.
-
Stephen A, Lui F. Brief Psychotic Disorder. [Updated 2023 Jun 25]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK539912/
-
World Health Organization. (2022). Schizophrenia. https://www.who.int/news-room/fact-sheets/detail/schizophrenia
-
National Institute of Mental Health. (2024). Bipolar disorder. U.S. Department of Health and Human Services, National Institutes of Health. https://www.nimh.nih.gov/health/publications/bipolar-disorder
-
Sit, Dorothy, et al. “A Review of Postpartum Psychosis.” Journal of Women’s Health, vol. 15, no. 4, May 2006, pp. 352–68. DOI.org (Crossref), https://doi.org/10.1089/jwh.2006.15.352.
-
Understanding Psychosis - National Institute of Mental Health (NIMH). https://www.nimh.nih.gov/health/publications/understanding-psychosis. Accessed 10 Apr. 2025.
-
Kane JM, Kishimoto T, Correll CU. Non-adherence to medication in patients with psychotic disorders: epidemiology, contributing factors and management strategies. World Psychiatry. 2013 Oct;12(3):216-26. doi: 10.1002/wps.20060. PMID: 24096780; PMCID: PMC3799245.
-
Jameel HT, Panatik SA, Nabeel T, Sarwar F, Yaseen M, Jokerst T, Faiz Z. Observed Social Support and Willingness for the Treatment of Patients with Schizophrenia. Psychol Res Behav Manag. 2020 Feb 25;13:193-201. doi: 10.2147/PRBM.S243722. PMID: 32158288; PMCID: PMC7049275.
-
Gumley, A., & Schwannauer, M. (2006). Staying well after psychosis: A cognitive interpersonal approach to emotional recovery and relapse prevention. Wiley.
-
National Institute of Mental Health. (2023). Understanding psychosis. U.S. Department of Health and Human Services, National Institutes of Health. https://www.nimh.nih.gov/health/publications/understanding-psychosis
-
Wong HH, Yong YH, Shahwan S, Cetty L, Vaingankar J, Hon C, Lee H, Loh C, Abdin E, Subramaniam M. Case management in early psychosis intervention programme: Perspectives of clients and caregivers. Early Interv Psychiatry. 2019 Jun;13(3):598-603. doi: 10.1111/eip.12534. Epub 2017 Dec 14. PMID: 29239115; PMCID: PMC6635736.
-
NAMI. “Emotional Recovery from Psychosis: Trusting and Believing in Yourself Again.” NAMI, 7 Dec. 2022, https://www.nami.org/Blogs/NAMI-Blog/December-2022/Emotional-Recovery-from-Psychosis-Trusting-and-Believing-in-Yourself-Again.
-
News, Neuroscience. “New Insight Into Brain’s Attempts at Psychosis Recovery.” Neuroscience News, 16 Feb. 2022, https://neurosciencenews.com/psychosis-brain-20078/.
Our Promise
How Is Recovery.com Different?
We believe everyone deserves access to accurate, unbiased information about mental health and recovery. That’s why we have a comprehensive set of treatment providers and don't charge for inclusion. Any center that meets our criteria can list for free. We do not and have never accepted fees for referring someone to a particular center. Providers who advertise with us must be verified by our Research Team and we clearly mark their status as advertisers.
Our goal is to help you choose the best path for your recovery. That begins with information you can trust.









