How Do I Know if I Need Mental Health and Addiction Treatment?



Caroline Beidler, MSW is an author, speaker, and the Managing Editor of Recovery.com. She writes about topics related to addiction, mental health, and trauma recovery, informed by her personal experience and professional expertise.

Dr. Mala, is the Chief Clinical Officer at Recovery.com, where she develops impartial and informative resources for people seeking addiction and mental health treatment.




Caroline Beidler, MSW is an author, speaker, and the Managing Editor of Recovery.com. She writes about topics related to addiction, mental health, and trauma recovery, informed by her personal experience and professional expertise.

Dr. Mala, is the Chief Clinical Officer at Recovery.com, where she develops impartial and informative resources for people seeking addiction and mental health treatment.
If you’re reading this, you might be wondering, “Do I need help?”
That question alone takes courage, and it could be the most important first step in your healing journey.
Acknowledging the need for mental health or addiction treatment is not a sign of weakness. It’s a sign of wisdom. It means you know something isn’t right, and that you might be open to change.
Change is where healing begins.
When stress, anxiety, substance use, or feeling lost becomes overwhelming, it can be hard to know if you need professional help. This guide will help you recognize when it’s time to seek treatment and how to take that first step.
Recognizing Signs and Symptoms
Recognizing when you need help is the first, and often hardest, step toward healing.
It can be challenging to recognize the signs and symptoms of addiction and mental health conditions.1 But, behavioral health experts say there are common indicators. Often, our loved ones or family members are the first to notice and point out changes.
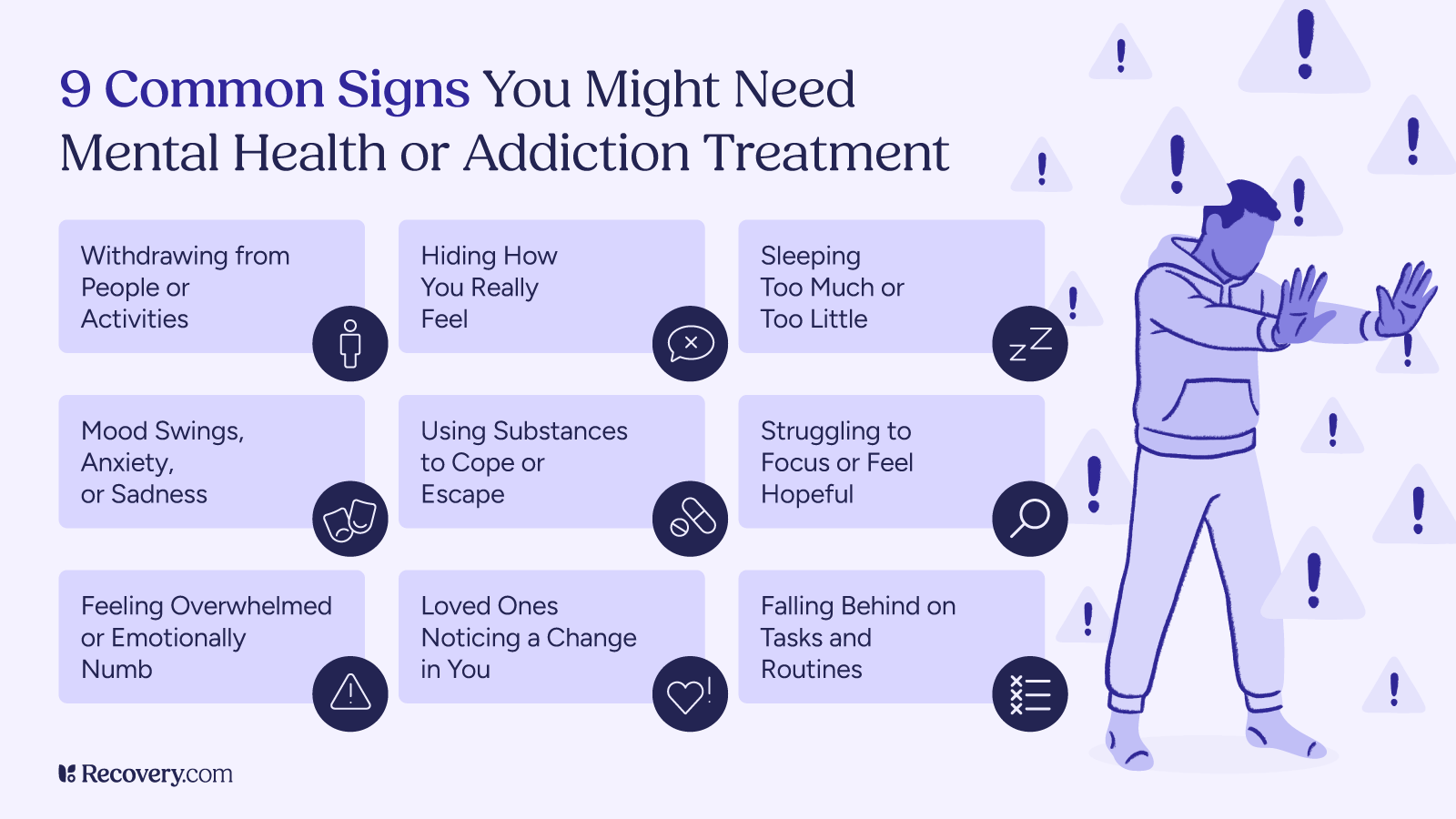
These warning signs typically fall into three main categories that affect how we act, feel, and function physically.
Behavioral, Emotional, and Physical Indicators
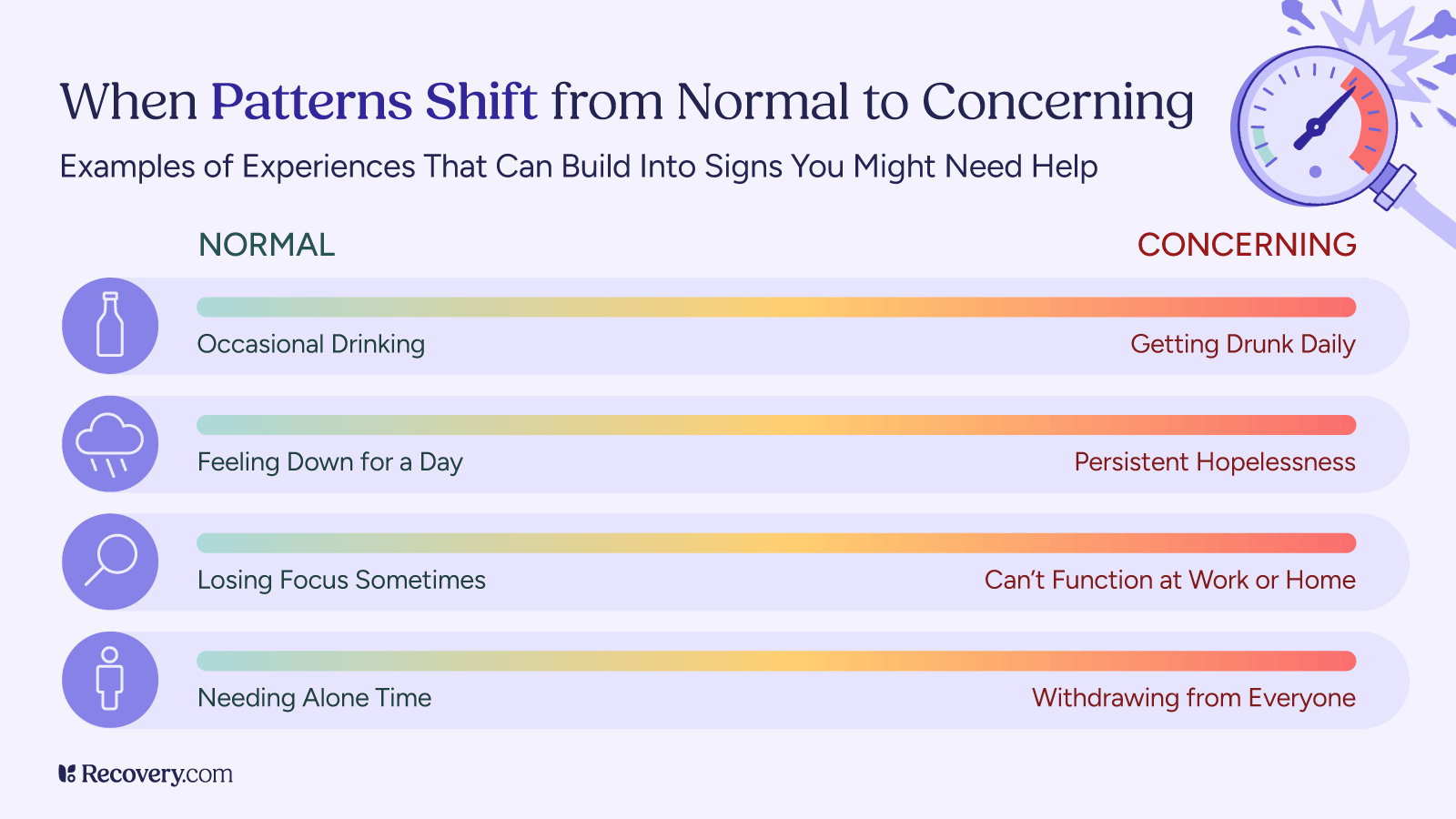
Mental health and substance use issues often show up in subtle ways at first. You might not even realize how much they affect your life until someone else points it out—or until it starts interfering with your peace. Over time, consequences can get more severe and start to impact your quality of life.2
Here are some red flags to watch for:
- Withdrawing from friends, family, or favorite activities
- Ongoing mood swings, anxiety, irritability, or deep sadness
- Trouble sleeping, or sleeping too much
- Significant weight loss or gain
- Neglecting hygiene
- Using substances (like alcohol, drugs, food, or even social media) to escape
- Difficulty concentrating, staying motivated, or feeling hopeful
- Feeling like life is overwhelming or not worth living
If you’re experiencing several of these symptoms, your mind and body may be signaling that it’s time for support.
Self-Assessment Tools and Questions
If you’ve noticed potential warning signs, specific assessment tools can help you evaluate whether your symptoms warrant professional attention.
Note: These assessments should not replace a formal diagnosis, but your results may indicate whether it’s a good idea to seek a clinical evaluation. If your answers point to possible signs of addiction or mental health concerns, consider speaking with a professional for support or further evaluation.
Clinical Screening Tools for Self-Assessment
Healthcare providers commonly use the following evidence-based screening tools in treatment settings, but they’re also available for self-assessment.3
GAD-7: Generalized Anxiety Disorder 7-Item Scale
What it’s for: Screens for generalized anxiety disorder and assesses severity. Also effective at detecting panic disorder, social anxiety disorder, and PTSD.
How it’s used: Rate how often you’ve been bothered by anxiety symptoms over the past 2 weeks. Takes 2-3 minutes to complete.
Sample questions:
Over the last 2 weeks, how often have you been bothered by the following problems?
- Feeling nervous, anxious, or on edge
- Not being able to stop or control worrying
- Trouble relaxing
Where to find it: The GAD-7 is available online or through your healthcare provider.4
PHQ-9: Patient Health Questionnaire-9
What it’s for: Screens for depression based on DSM-5 criteria and assesses severity, including suicidal ideation.
How it’s used: Rate how often symptoms have affected you over the last 2 weeks. Takes 3-5 minutes to complete.
Sample questions:
Over the last 2 weeks, how often have you been bothered by the following problems?
- Little interest or pleasure in doing things
- Feeling down, depressed, or hopeless
- Thoughts that you would be better off dead or hurting yourself
Where to find it: The PHQ-9 is available online or through your healthcare provider.5
CAGE Questionnaire (Cut Down, Annoyed, Guilty, Eye-Opener)
What it’s for: Brief screening tool to identify alcohol misuse.
How it’s used: Four yes-or-no questions that take about one minute to complete.
Sample questions:
- Have you ever felt you should cut down on your drinking?
- Have people annoyed you by criticizing your drinking?
- Have you ever felt guilty about your drinking?
- Have you ever had a drink first thing in the morning to steady your nerves or get rid of a hangover?
Where to find it: The CAGE Questionnaire is available online or through your healthcare provider.6
These self-assessment tools offer a quick, confidential way to evaluate whether you may benefit from professional support. While they don’t provide a diagnosis, they can identify concerning patterns and help guide your next steps.
Of course, taking an honest self-assessment requires acknowledging that there might actually be a problem, which isn’t always easy.
The Role of Denial and Minimization
Let’s be honest. It can be easy to talk yourself out of needing help.
Maybe you have said things like:
- “It’s not that bad.”
- “I can handle this on my own.”
- “Other people have it worse.”
Minimizing or denying a problem is a common part of struggling with addiction or mental health concerns. It’s a way the mind tries to protect itself from pain by pretending things are fine. But most people underestimate how much their struggles are actually affecting their lives. Denial helps you feel in control, while minimizing sounds like “It’s not that bad” or “I can stop anytime”—but both can keep you from getting help when you need it most.
These thought patterns can delay help until a crisis occurs. But it’s important to remember that you don’t need to be in crisis to deserve support.
When “Functioning” Doesn’t Mean “Healthy”
You don’t need to lose your job, home, or relationships to require treatment. Many people with mental health or substance use disorders are still meeting their responsibilities at work or school. This is known as “high functioning.”7
Busting the Myth of the High-Functioning Addict
Not everyone struggling with addiction:
- Drinks or uses in the morning
- Gets a DUI
- Misses work regularly
Not everyone with a mental health condition:
- Experiences suicidal ideation
- Has difficulty in social situations
- Needs hospitalization
These things can and do happen for many people. However, addiction and mental illness look different for everyone. “Functioning” doesn’t mean your mental well-being is intact. High-functioning alcoholism, drug addiction, anxiety, or depression can fly under the radar for years. But that doesn’t mean you couldn’t benefit from treatment to improve your physical, mental, or spiritual well-being.
What Loved Ones Might Notice First
Sometimes, the people closest to us can see the signs before we’re ready to. It’s not because they’re trying to judge, it’s because they care. They know your usual patterns, and when something shifts, they notice.
Here are some common changes or warning signs loved ones or others closest to you, like family members or employers, may notice:8
- A drop in mood or energy: You may seem tired, irritable, or not yourself—even if you don’t realize it.
- Changes in routine or motivation: Maybe you’re skipping work, sleeping all day, or losing interest in things you used to love.
- Avoiding responsibilities or isolating: Pulling away from family, missing events, or spending long hours alone can be a red flag.
- Unusual behavior or secrecy: Loved ones might notice you’re being vague, avoiding eye contact, or hiding parts of your day.
- Increased substance use: They may comment on how much you’re drinking or using—and how it’s affecting your mood or relationships.
- Emotional outbursts or numbness: Whether you’re snapping easily or seem checked out, they may sense something’s off emotionally.
Sometimes, these observations come as gentle concern. Other times, they may sound like frustration. Either way, don’t dismiss what your loved ones say, even if it’s hard to hear.
Why this matters:
When you’re in the middle of a mental health or addiction struggle, your view can get clouded. You might not notice how your habits or emotions have shifted. That’s why outside perspectives are valuable—they help you see what you might be missing.
What to do next:
- Ask someone you trust: “Have you noticed any changes in me lately?”
- Listen without defending. Just take it in with an open heart.
- If several people have expressed concern, it’s worth exploring.
Remember: A loved one noticing a change in you or family members sharing a concern isn’t an accusation. It’s an invitation to check in with yourself and consider if help could make things better. Reaching out for support, including peer support, can be another helpful way to bring other people into what is going on in your life.
Next Steps if You’re Unsure

If you’re still unsure whether you need help, consider talking to a mental health professional or health care provider. A diagnostic evaluation typically includes:
- A review of your medical history
- A mental health screening
- Questions about alcohol use disorder, drug use, trauma, and mood
- Referral to treatment programs, psychotherapy, or support groups
These assessments can be conducted through outpatient mental health services, inpatient programs, or telehealth.
If you’ve read this far, something inside you is reaching for hope—and that matters.
You don’t need to have it all together to ask for help. You just need to be willing to take one small step.
No matter where you are in the process, you’re not alone. Recovery is possible and there’s a community here to help you take the next step. Find qualified addiction treatment programs in your area that offer personalized care when you need it most.
FAQs
-
What Is a Substance Use Disorder? https://www.psychiatry.org:443/patients-families/addiction-substance-use-disorders/what-is-a-substance-use-disorder. Accessed 20 June 2025.
-
Hohls JK, König HH, Quirke E, Hajek A. Anxiety, Depression and Quality of Life-A Systematic Review of Evidence from Longitudinal Observational Studies. Int J Environ Res Public Health. 2021 Nov 16;18(22):12022. doi: 10.3390/ijerph182212022. PMID: 34831779; PMCID: PMC8621394.
-
Center for Substance Abuse Treatment. A Guide to Substance Abuse Services for Primary Care Clinicians. Rockville (MD): Substance Abuse and Mental Health Services Administration (US); 1997. (Treatment Improvement Protocol (TIP) Series, No. 24.) Chapter 2—Screening for Substance Use Disorders. Available from: https://www.ncbi.nlm.nih.gov/books/NBK64820/
-
"GAD-7 Anxiety." Anxiety and Depression Association of America. https://adaa.org/sites/default/files/GAD-7_Anxiety-updated_0.pdf
-
"PATIENT HEALTH QUESTIONNAIRE-9 (PHQ-9)." APA. https://www.apa.org/depression-guideline/patient-health-questionnaire.pdf
-
"CAGE Substance Abuse Screening Tool." Johns Hopkins Medicine. https://portal.ct.gov/-/media/dph/maternal-mortality/cage-substance-screening-tool.pdf
-
Glauser W. "High-functioning addicts": intervening before trouble hits. CMAJ. 2014 Jan 7;186(1):19. doi: 10.1503/cmaj.109-4667. Epub 2013 Dec 2. PMID: 24295863; PMCID: PMC3883816.
-
"10 Warning Signs." National Alliance on Mental Illness (NAMI), https://www.nami.org/Press-Media/Press-Releases/2015/10-Warning-Signs. Accessed 20 June 2025.
-
"Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR)." Psychiatry Online. https://www.psychiatryonline.org/dsm
Our Promise
How Is Recovery.com Different?
We believe everyone deserves access to accurate, unbiased information about mental health and recovery. That’s why we have a comprehensive set of treatment providers and don't charge for inclusion. Any center that meets our criteria can list for free. We do not and have never accepted fees for referring someone to a particular center. Providers who advertise with us must be verified by our Research Team and we clearly mark their status as advertisers.
Our goal is to help you choose the best path for your recovery. That begins with information you can trust.










