What Is Wet Brain? 5 Important Truths That Could Prevent Brain Damage



Hannah is a holistic wellness writer who explores post-traumatic growth and the mind-body connection through her work for various health and wellness platforms. She is also a licensed massage therapist who has contributed meditations, essays, and blog posts to apps and websites focused on mental health and fitness.

Dr. Mala, is the Chief Clinical Officer at Recovery.com, where she develops impartial and informative resources for people seeking addiction and mental health treatment.




Hannah is a holistic wellness writer who explores post-traumatic growth and the mind-body connection through her work for various health and wellness platforms. She is also a licensed massage therapist who has contributed meditations, essays, and blog posts to apps and websites focused on mental health and fitness.

Dr. Mala, is the Chief Clinical Officer at Recovery.com, where she develops impartial and informative resources for people seeking addiction and mental health treatment.
Table of Contents
- 1. Wernicke-Korsakoff Syndrome Is a 2-Stage Brain Condition
- 2. Alcohol Disrupts Essential Vitamin B1 Absorption
- 3. It’s Easy to Overlook Early Warning Signs
- 4. Certain Risk Factors Increase Your Vulnerability
- 5. Prompt Treatment Can Reverse Some Brain Damage
- Can Wet Brain Be Reversed?
- Getting Help for Alcohol Use Disorder
- FAQs
If you’ve heard the term “wet brain,” you might be wondering what it means. Put simply, wet brain happens when long-term alcohol consumption causes a severe shortage of vitamin B1 in the body, which then damages the brain. It’s medically known as Wernicke-Korsakoff syndrome, and it can affect basic things like memory, balance, and mental function.
You don’t have to be a heavy drinker to develop wet brain—it can happen to anyone who regularly drinks alcohol. The good news is that getting help early can protect your brain from the effects of alcohol. In this guide, we’ll walk you through the warning signs, risk factors, treatment options, and the path to recovery.
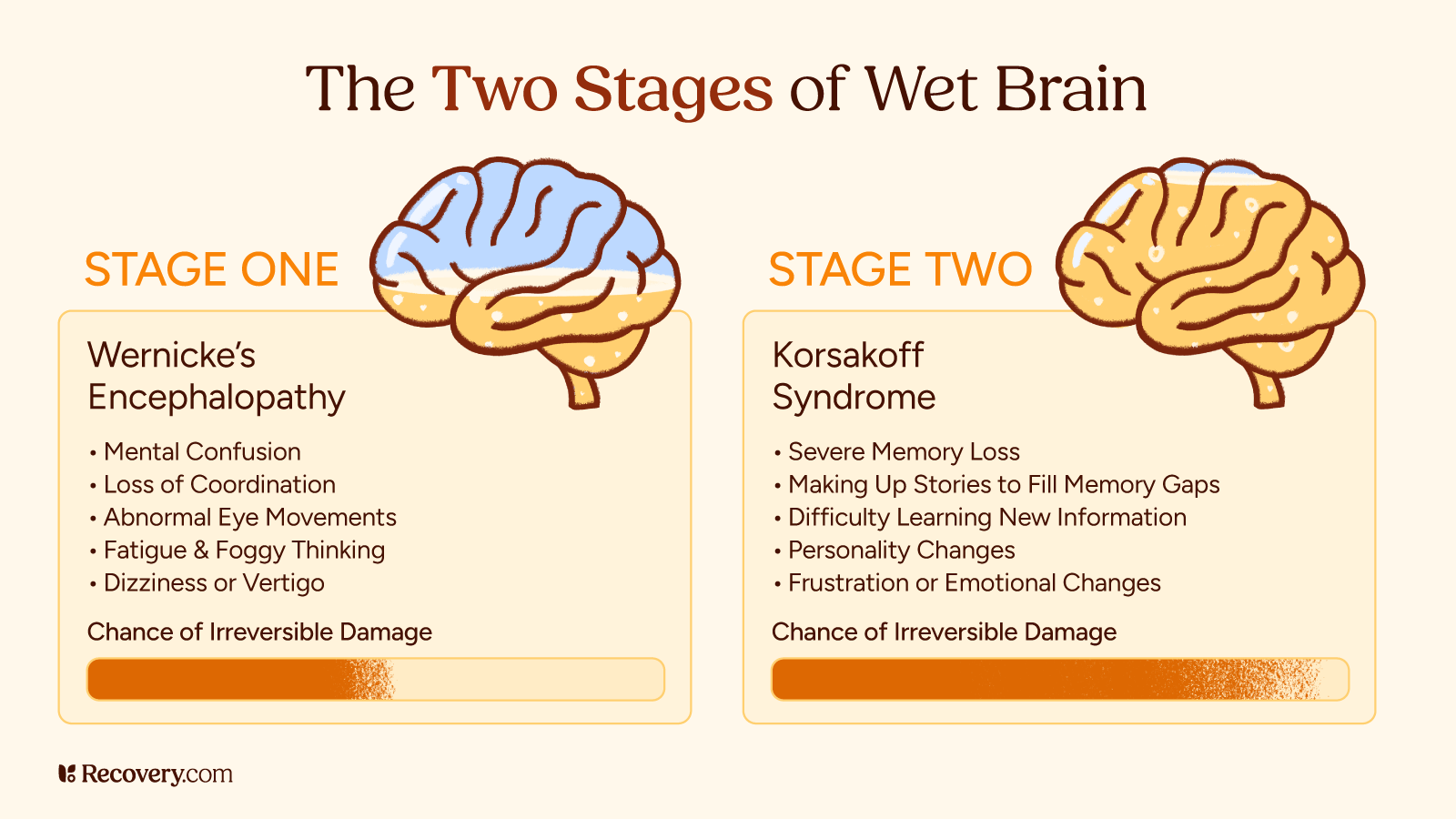
1. Wernicke-Korsakoff Syndrome Is a 2-Stage Brain Condition
Wernicke-Korsakoff syndrome (WKS),1 commonly known as wet brain, is actually 2 separate conditions that often occur together. You can think of it as a 2-stage problem that affects your brain.
The first stage, called Wernicke’s encephalopathy, happens when your body doesn’t have enough vitamin B1 (thiamine).2 Your brain needs this vitamin to work properly. Without it, your brain tissue can become damaged, especially in areas that control balance, eye movements, and basic mental functions.
The second stage, Korsakoff syndrome, is a neurological disorder that can develop if Wernicke’s encephalopathy isn’t treated quickly. The main traits of this phase are memory impairment and difficulty learning new information. You might find yourself forgetting recent conversations or having trouble remembering how to do familiar tasks.
The nickname “wet brain” comes from the way this condition affects brain tissue. When someone has severe thiamine deficiency,3 it can cause swelling in the brain and damage brain cells, making brain tissue appear “wet” when examined. While this term isn’t a medical one, it’s widely used as it helps people understand the physical nature of the condition.
Both stages of wet brain are serious medical conditions that need immediate attention. Without treatment, the damage can become permanent. But catching it early and getting proper medical care can make a big difference in your recovery.
2. Alcohol Disrupts Essential Vitamin B1 Absorption
Alcohol can lead to wet brain in several ways, but it all comes down to your thiamine levels. When you drink alcohol regularly, it becomes harder for your body to absorb enough of this essential vitamin. As a result, your brain struggles to process glucose, which affects its ability to function properly.
Here’s what happens:
First, alcohol blocks your body’s ability to absorb vitamin B1 from food.4 Even if you’re eating healthy foods, alcohol can prevent your body from using this vitamin properly.
Second, many people who drink heavily often don’t eat regular, nutritious meals. They might skip meals or choose foods that aren’t nutrient-dense. This means they’re getting less essential vitamins and minerals—including B1—than their body needs.
Finally, alcohol misuse can cause frequent vomiting and diarrhea, which further depletes your body’s vitamin stores.
This is why healthcare providers often give vitamin B1 supplements to people in addiction treatment for alcohol use disorder:5 People who have been drinking alcohol for a long time are usually depleted of this essential vitamin.

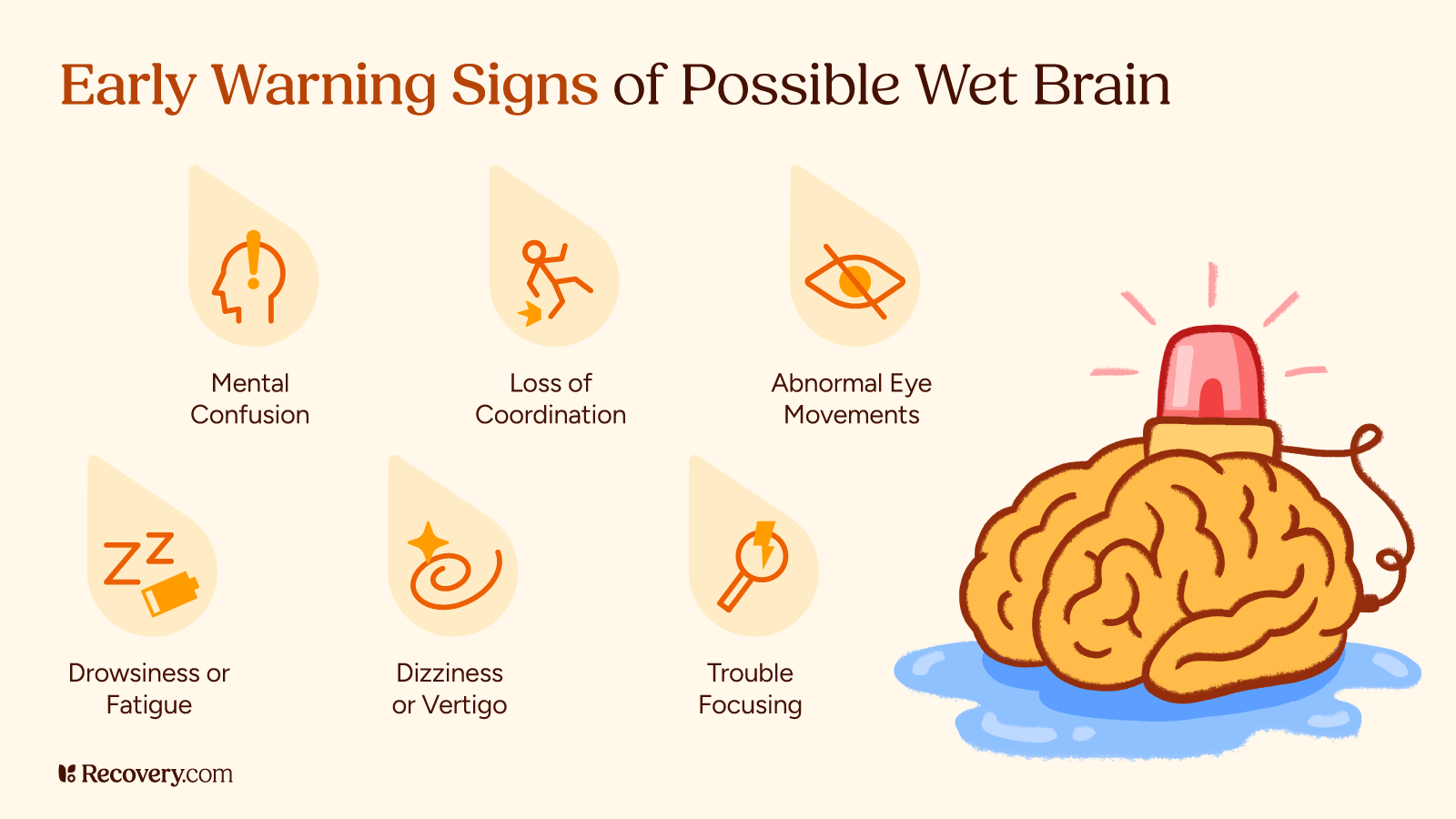
3. It’s Easy to Overlook Early Warning Signs
Wet brain develops in stages, and knowing the warning signs can help you prevent permanent brain damage. The symptoms of Wernicke’s encephalopathy might start subtly but can quickly become serious. Let’s look at what happens in each stage.
Early Symptoms
The early signs of wet brain syndrome can come on suddenly and might include:
- Low blood pressure
- Feeling confused,6 foggy, or unable to think clearly
- Problems with muscle coordination and balance—you might feel unsteady on your feet or walk with an unusual gait
- Changes in your eyes or vision, such as double vision, drooping eyelids, or eye movements you can’t control
- Feeling very tired or drowsy during the day
- Having trouble paying attention or staying focused
- Feeling dizzy or having vertigo, like the room is spinning
If you notice any of these signs, get medical help as soon as possible—early treatment can prevent more serious problems from developing.
What are the most commonly overlooked early warning signs of wet brain that people should watch for in a loved one with alcohol use disorder?

Later-Stage Symptoms
If early signs aren’t treated, you can develop symptoms of Korsakoff syndrome (sometimes called Korsakoff psychosis). In more severe cases, these symptoms can be long-lasting:
- Significant memory loss, especially trouble making new memories—you might forget conversations that just happened or places you just visited
- Making up stories to fill in memory gaps without realizing you’re doing it (this is called confabulation)
- Difficulty learning new information or skills
- Personality changes—you might seem like a different person to friends and family
- Problems understanding or following conversations
- Feeling frustrated or irritable more often than usual
The good news is that getting help at any stage can make a difference. While some symptoms might be permanent if left untreated, proper medical care may help improve some symptoms and can stop the condition from getting worse.
4. Certain Risk Factors Increase Your Vulnerability
While wet brain is most common in people who drink alcohol regularly, other factors can increase your risk. Wet brain is more likely to affect:
- People who drink alcohol frequently, especially those who might skip meals or not eat regularly
- Anyone with an eating disorder, poor diet, or malnutrition
- People who have had gastric bypass surgery
- Those with health conditions that affect their thiamine absorption
- People experiencing homelessness who might not have access to regular, nutritious meals
- Anyone undergoing cancer treatment that affects their ability to eat or absorb nutrients
- People with severe morning sickness during pregnancy
You can help prevent wet brain by:
- Stopping or reducing your alcohol intake (or getting help for alcohol addiction if you’re having trouble stopping on your own)
- Eating a nutrient-rich, balanced diet
- Taking thiamine supplements or other vitamins as recommended by your doctor
- Getting medical help if you’re having trouble controlling your drinking
- Seeking treatment for eating disorders or other conditions that cause poor nutrition
5. Prompt Treatment Can Reverse Some Brain Damage
When someone shows signs of wet brain, doctors typically take these steps.
First, they’ll do a thorough medical exam, looking specifically at:
- Your balance and way of walking
- Your eye movements
- Your memory and thinking abilities
- Your nutrition status
They might also run blood teststo check your vitamin B1 levels and order brain imaging tests7 like an MRI to look for neurological changes.
Treatment usually involves:
- Immediate vitamin B1 replacement, usually through an IV at first
- Making sure you’re getting proper nutrition
- Treating any other medical issues
- Supporting you to safely stop drinking
What continuing care strategies are most effective for supporting long-term recovery in people with Wernicke-Korsakoff syndrome?
Can Wet Brain Be Reversed?
The possibility of recovery from wet brain depends largely on when you get treatment. Here’s what you can expect:
Early Stage (Wernicke’s encephalopathy):
- Many symptoms can improve or go away completely with quick treatment
- Vision impairment and balance issues often get better within days or weeks
- The sooner you get treatment, the more it will help your recovery
Later Stage (Korsakoff syndrome):
- Some symptoms might be permanent, but getting treatment can stop them from getting worse
- About 25% of people recover completely
- About half show significant improvement with treatment
- The remaining 25% may have lasting symptoms that need long-term support
Even if some symptoms can’t be completely reversed, getting treatment can help you prevent further damage and improve your quality of life.
Getting Help for Alcohol Use Disorder
If you’re worried about your drinking or think you might be developing symptoms of wet brain, know that help is available—and it works. Treatment options include:
- Medical detox programs to ease alcohol withdrawal and help you stop drinking safely
- Inpatient or outpatient rehab programs
- Individual counseling and group therapy
- Support groups like AA or SMART Recovery
- Medications that can help reduce alcohol cravings
Don’t wait until alcohol abuse affects your physical and mental health—start reclaiming your wellness today. Find accredited alcohol treatment centers near you that can help you (or your loved one) safely stop drinking and prevent serious complications like wet brain.
FAQs
Q: How long does it take to develop wet brain?
A: There’s no set timeline—it varies from person to person. Some people develop symptoms after months of heavy drinking, while others might drink for years before showing signs. The key factor isn’t just how long someone drinks, but how severely their body becomes depleted of vitamin B1.
Q: Is alcoholic dementia the same as wet brain?
A: While similar, they’re different conditions. Alcoholic dementia develops gradually from long-term alcohol use affecting the brain in various ways. Wet brain (Wernicke-Korsakoff syndrome) specifically results from severe vitamin B1 deficiency and has more distinct stages and symptoms.
Q: What is the life expectancy of someone with wet brain?
A: Without treatment, wet brain can be life-threatening. However, with proper medical care and stopping alcohol use, many people live normal lifespans. Life expectancy depends largely on when treatment begins and how well you follow your treatment program.
-
1. Wernicke-Korsakoff Syndrome: MedlinePlus Medical Encyclopedia. https://medlineplus.gov/ency/article/000771.htm. Accessed 1 May 2025.
-
2. Thiamin: MedlinePlus Medical Encyclopedia. https://medlineplus.gov/ency/article/002401.htm
-
3. Martin PR, Singleton CK, Hiller-Sturmhöfel S. The role of thiamine deficiency in alcoholic brain disease. Alcohol Res Health. 2003;27(2):134-42. PMID: 15303623; PMCID: PMC6668887.
-
4. Alcohol Related Thiamine Deficiency - Alcohol and Drug Foundation. https://adf.org.au/insights/alcohol-related-thiamine-deficiency/. Accessed 1 May 2025.
-
5. Dervaux A, Laqueille X. Le traitement par thiamine (vitamine B1) dans l’alcoolodépendance [Thiamine (vitamin B1) treatment in patients with alcohol dependence]. Presse Med. 2017 Mar;46(2 Pt 1):165-171. French. doi: 10.1016/j.lpm.2016.07.025. Epub 2016 Nov 3. PMID: 27818067.
-
6. Osiezagha K, Ali S, Freeman C, Barker NC, Jabeen S, Maitra S, Olagbemiro Y, Richie W, Bailey RK. Thiamine deficiency and delirium. Innov Clin Neurosci. 2013 Apr;10(4):26-32. PMID: 23696956; PMCID: PMC3659035.
-
7. Sullivan EV, Pfefferbaum A. Neuroimaging of the Wernicke-Korsakoff syndrome. Alcohol Alcohol. 2009 Mar-Apr;44(2):155-65. doi: 10.1093/alcalc/agn103. Epub 2008 Dec 9. PMID: 19066199; PMCID: PMC2724861.
Our Promise
How Is Recovery.com Different?
We believe everyone deserves access to accurate, unbiased information about mental health and recovery. That’s why we have a comprehensive set of treatment providers and don't charge for inclusion. Any center that meets our criteria can list for free. We do not and have never accepted fees for referring someone to a particular center. Providers who advertise with us must be verified by our Research Team and we clearly mark their status as advertisers.
Our goal is to help you choose the best path for your recovery. That begins with information you can trust.