What Is Binge Eating?



Sarah holds a B.A. in Psychology from the University of Wisconsin-Madison where she was part of a psycho-social research lab. She is the Content Manager and Editor at Recovery.com, creating informational video resources on behavioral health.

Dr. Mala, is the Chief Clinical Officer at Recovery.com, where she develops impartial and informative resources for people seeking addiction and mental health treatment.




Sarah holds a B.A. in Psychology from the University of Wisconsin-Madison where she was part of a psycho-social research lab. She is the Content Manager and Editor at Recovery.com, creating informational video resources on behavioral health.

Dr. Mala, is the Chief Clinical Officer at Recovery.com, where she develops impartial and informative resources for people seeking addiction and mental health treatment.
Binge eating involves recurring episodes of eating large amounts of food in a short amount of time. Recognizing the signs of binge eating is important because it has physical, mental, and societal effects.
Your mental and physical health can deteriorate from binging episodes. Those who struggle with binge eating often experience intense guilt, shame, and distress, which can negatively impact self-esteem and well-being. Usually there’s a deeper root cause, like something emotionally-driven, behind your binging episodes. And eating large amounts of food can lead to significant weight gain and related health problems.
Caring about your health, and taking steps to improve it, is essential for your well-being. Prioritizing your health can empower you to lead a fulfilling life and positively impact your loved ones and communities.
Defining Binge Eating
The DSM-51 defines binge eating disorder (BED) as “eating, in a discrete amount of time (e.g., within any two hour period), an amount of food that is definitely larger than what most people would eat in a similar period of time under similar circumstances.”
Often, those with BED feel a lack of control when they’re binging. And sometimes, they’ll eat alone because they’re embarrassed or disgusted by how much they eat.
BED occurs frequently. Overeating to the point of feeling uncomfortably full may be distinct from BED, as the episodes do not occur as often. If these episodes are followed by purging behaviors such as self-induced vomiting or excessive laxative use, you may be diagnosed with bulimia nervosa.
Symptoms and Signs of Binge Eating
Common behavioral indicators of BED include:
- Eating faster than normal during an episode
- Eating until uncomfortably full
- Eating a large amount of food, even when you’re not hungry
- Feeling ashamed of your binge eating, and often hiding it from others
- Often choosing to eat high-calorie foods that are rich in fats and sugars
- Hoarding food
Emotional signs of BED include:
- Feeling a loss of control over your eating
- Emotional distress
- Emotional numbing
- Obsession with weight/body image
Causes and Risk Factors
While no one thing leads to binge eating disorder, various influences can trigger its onset. That’s why looking at this disorder with a multifaceted approach is so important.
Biological Factors
While you may think these eating patterns are something you can easily stop on your own, BED mirrors the neurobiology of substance use disorder.3 Palatable foods, along with drugs and alcohol, can change your brain.
Eating sugary and fatty foods increases endogenous opioid activity in the brain, and over time this binging cycle can alter the opioid system, just like with substance addiction. Additionally, activating the dopamine system can temporarily relieve stress, and eating these foods can do just that. However, this can lead to food, or substance, addiction which can also change your brain chemistry.
The gut-brain axis is the bidirectional communication between the gastrointestinal system and the brain.4 Emerging research suggests that gut microbiota composition and function may influence food cravings, mood, and eating behaviors, potentially contributing to binge eating tendencies.
Emotional Triggers
Emotional triggers can play a role in BED, too. Those with binge eating disorder often reach for food when they’re feeling uncomfortable emotions like stress, loneliness, and sadness. This happens because you think you’re craving food, when in reality you’re lacking something emotional, like security, control, warmth, excitement, or love. Unfortunately, food does not compensate for these non-negotiable emotional needs.
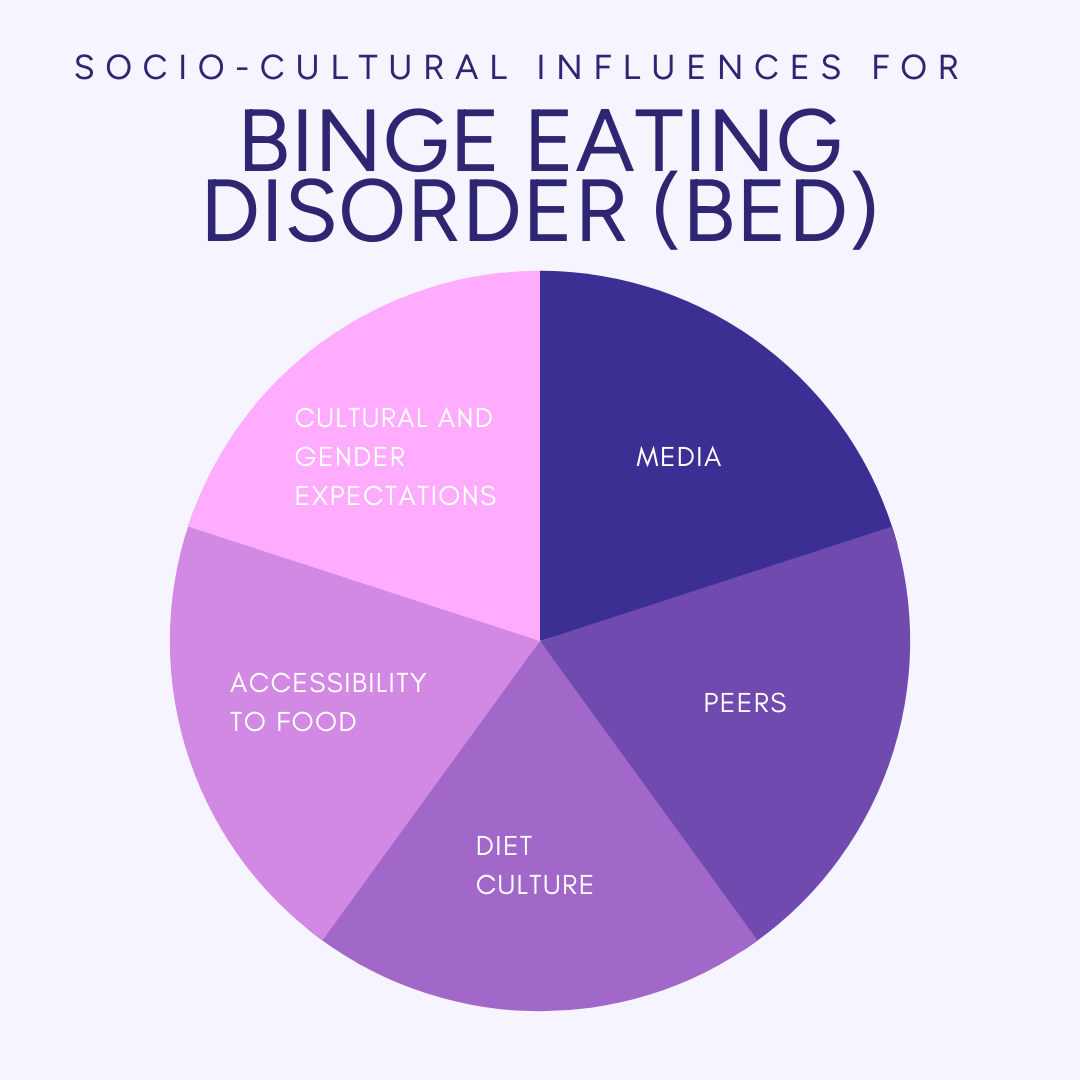
Socio-cultural Influences
Socio-cultural influences play a significant role in shaping body image ideals, dieting behaviors, and the development of binge eating tendencies. Some key socio-cultural factors that contribute to this include:
- Media: Thin, idealized bodies we see in the media contribute to unrealistic beauty standards.
- Peers: Peer pressure, comparisons, and social acceptance can contribute to body dissatisfaction and a desire to conform to certain appearance standards.
- Diet culture: This culture claims thinness equals health and moral superiority. It emphasizes strict dieting, weight loss, and the pursuit of an “ideal” body shape.
- Accessibility to food: Limited access to affordable, nutritious foods may lead to reliance on cheap, energy-dense foods, which can contribute to weight gain and disordered eating patterns.
- Cultural and gender expectations: Cultural ideals and gender expectations can influence body image and eating behaviors differently across societies. For example, certain cultures may value larger body sizes as a symbol of beauty and fertility, while others may prioritize thinness.
Consequences of Binge Eating
Binge eating can have significant physical health implications, particularly when it leads to obesity and related medical conditions. It can result in:
- Type 2 diabetes
- Cardiovascular disease
- Gastrointestinal problems
- Sleep apnea
- Joint problems
- Respiratory issues
Aside from physical health, BED can take a toll on you emotionally. There is a relationship between binge eating and anxiety and depression because binging is often used as an escape from these complicated feelings. You may also experience low self-esteem and guilt because of your eating habits.
Binge eating can impact your overall quality of life. It can strain relationships because your embarrassment could lead you to isolate yourself or avoid social situations that involve food. It could also impact your work or hobbies because of the fatigue, reduced concentration, and emotional distress that comes with BED.
Addressing binge eating through treatment and support can help you improve your relationships, social life, and overall quality of life. Therapy, support groups, and developing positive coping mechanisms can promote a healthier relationship with food, enhance self-esteem, and facilitate meaningful connections with others.
Diagnosis and Treatment
According to the DSM-51, BED is diagnosed by
- Eating a larger than normal amount of food in a discrete period of time
- A lack of control during these binging periods
- 3 or more of the following:
- Eating more rapidly than normal
- Eating until feeling uncomfortably full
- Eating large amounts of food when not hungry
- Eating alone because of embarrassment when binging around others
- Feeling shame and depressed after binging
- Marked distress about the binging
- Episodes occurring 1+ times per week for 3+ months
- The binge eating not being followed by purging behaviors
If you think that you or someone you know may have BED, it is important to seek help from a healthcare professional. A proper diagnosis can guide the creation of your treatment plan, and early intervention can significantly improve outcomes and quality of life.
Therapy for BED
Cognitive behavioral therapy (CBT) is an effective treatment for binge eating disorder (BED).4 It addresses the underlying thoughts, emotions, and behaviors associated with binge eating. CBT aims to challenge and modify unhelpful thoughts and beliefs, and it helps you develop alternative coping strategies. It’s also beneficial for co-occurring disorders like anxiety or depression because CBT is a widely recognized treatment for many mental health disorders5.
Interpersonal therapy (IPT) is another evidence-based approach used for BED treatment. IPT focuses on addressing interpersonal issues and improving relationships to reduce binge eating behaviors. This could look like learning to cope with emotions like stress, sadness, or anger in healthier ways, in turn relying less on food as a way to deal with them.
Strategies for Coping with Binge Eating
While professional treatment is the most important component for recovery, building a healthy relationship with food and practicing mindful eating can help you along your journey.
This can look like paying attention to your body’s hunger and fullness cues, mindful eating where you slow down eating and pay attention to the food sensations, stocking your kitchen with nutritious foods, and striving for a flexible, non-restrictive approach to eating.
If your BED is triggered by stress, developing effective stress management techniques can help you navigate a trigger before the binge starts. This could be deep breathing exercises, getting adequate sleep, exercising, and positive self-talk.
Finally, seek support from friends, family, or support groups. Sharing your feelings and experiences with trusted individuals can provide comfort and perspective. And engaging in social activities and maintaining healthy relationships can also help reduce stress levels and manage your BED.
Prevention and Long-Term Management
Building a healthy relationship with food and your body is the best way to prevent BED. You can adopt balanced eating patterns that include a variety of nutrient-rich foods. There are no “good” and “bad” foods, all food is fuel. So allow yourself to have those treats without feeling guilty. Being unrestrictive can help you sustain a healthy diet.
BED develops not just because of your eating habits but also from your emotional well-being and coping strategies. Keeping yourself mentally healthy is just as important as being physically healthy. Find positive ways to cope with stress, boredom, or difficult emotions that do not involve turning to food. You can exercise, practice mindfulness, engage in creative outlets, or spend time with loved ones.
Ongoing self-care and self-compassion will be key in your journey. Set boundaries, validate your emotions, and create goals. Growth and being the best version of yourself doesn’t come from being your harshest critic. It comes from being your biggest supporter and talking to yourself like a best friend.
You Are Not Alone
Mental health struggles can feel isolating, but compassionate care is within reach. Browse our comprehensive list of inpatient mental health facilities and residential treatment centers for depression, trauma, anxiety, and more. Healing is possible; find mental health help for yourself or a loved one today.
FAQ
-
American Psychiatric Association. (2013). Desk reference to the diagnostic criteria from DSM-5 (R). American Psychiatric Association Publishing.
-
Mathes, W. F., Brownley, K. A., Mo, X., & Bulik, C. M. (2009). The biology of binge eating. Appetite, 52(3), 545–553. https://doi.org/10.1016/j.appet.2009.03.005
-
Appleton, J. (2018). The gut-brain axis: Influence of microbiota on mood and mental health. Integrative Medicine: A Clinician’s Journal, 17(4), 28–32. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6469458/
-
McElroy, S. L., Guerdjikova, A. I., Mori, N., Munoz, M. R., & Keck, P. E. (2015). Overview of the treatment of binge eating disorder. CNS Spectrums, 20(6), 546–556. https://doi.org/10.1017/S1092852915000759
-
Cognitive behavioural therapy (Cbt) | royal college of psychiatrists. (n.d.). Www.Rcpsych.Ac.Uk. Retrieved July 10, 2023. https://www.rcpsych.ac.uk/mental-health/treatments-and-wellbeing/cognitive-behavioural-therapy-(cbt)
Our Promise
How Is Recovery.com Different?
We believe everyone deserves access to accurate, unbiased information about mental health and recovery. That’s why we have a comprehensive set of treatment providers and don't charge for inclusion. Any center that meets our criteria can list for free. We do not and have never accepted fees for referring someone to a particular center. Providers who advertise with us must be verified by our Research Team and we clearly mark their status as advertisers.
Our goal is to help you choose the best path for your recovery. That begins with information you can trust.










