The Link Between Substance Abuse and Domestic Violence: Understanding and Breaking the Cycle



Hannah is a writer with a focus on holistic wellness. Her work explores post-traumatic growth and the connection between physical and mental health. In addition to writing for Recovery.com she has written meditations for NatureSpace and is a licensed massage therapist.



Hannah is a writer with a focus on holistic wellness. Her work explores post-traumatic growth and the connection between physical and mental health. In addition to writing for Recovery.com she has written meditations for NatureSpace and is a licensed massage therapist.
- Substance use is commonly associated with domestic violence.
- Domestic violence survivors are at a high risk of addiction.
- Seeking care for both addiction and DV-related trauma can help you break the cycle.
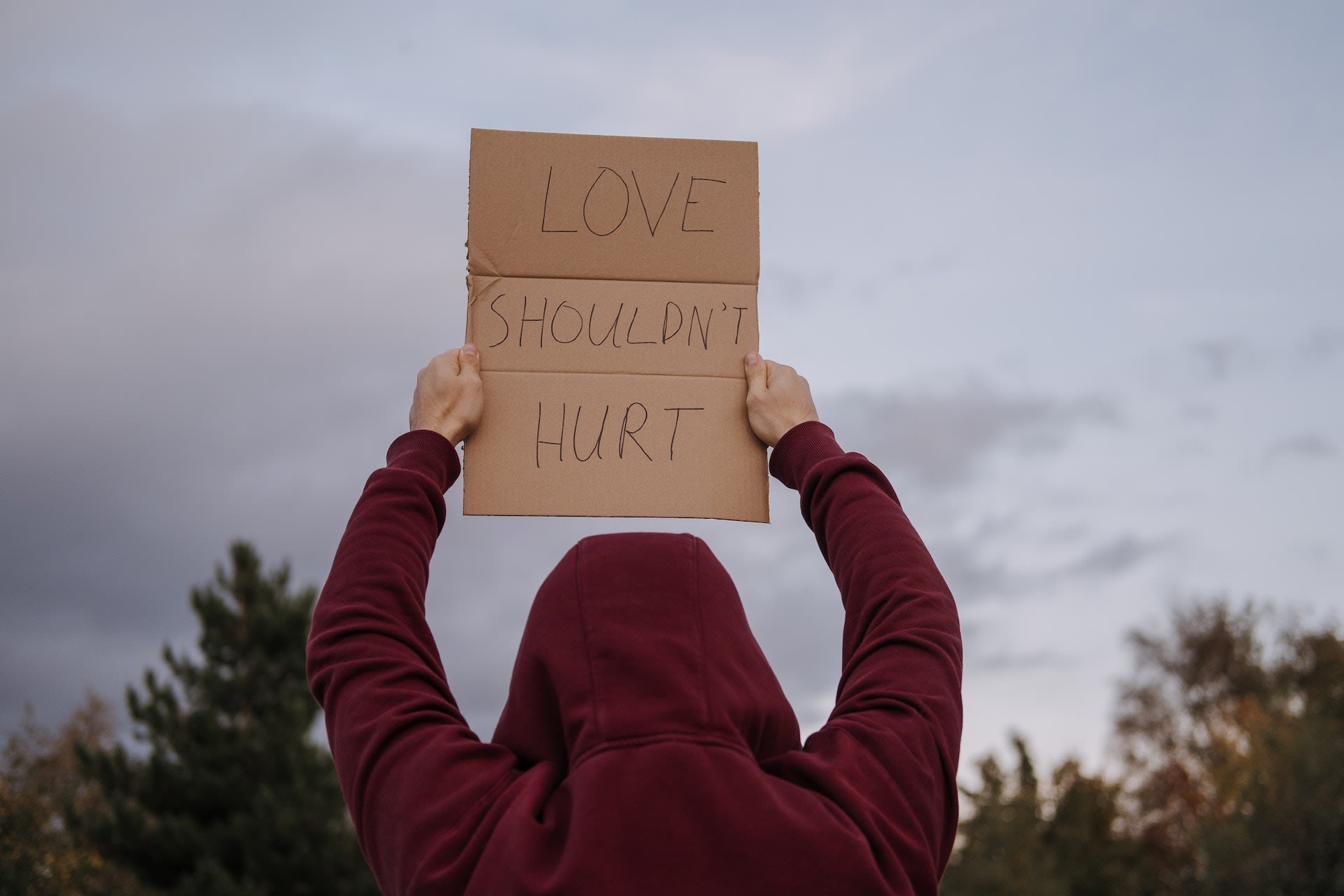
There’s a strong relationship between substance abuse and domestic violence. Abuse is traumatic, and its effects can follow you even after you end the relationship. Many people use drugs or alcohol to cope with that trauma, which can quickly lead to addiction. But addiction is traumatic, too. What starts as a coping mechanism might eventually compound the problem. When you’re ready to end this cycle, a rehab that treats trauma and addiction can help you move forward.
If you or someone in your life is experiencing domestic violence, you can call the National Domestic Violence Hotline at 1-800-799-SAFE (7233) to get immediate support.
What Is Domestic Violence?
Domestic violence is the intentional use of force by a family member, romantic partner, roommate, close friend, or other loved one. There’s a common myth that all abuse is physical assault. In reality, domestic violence can be much more subtle and complex. You don’t have to wait for it to escalate. Instead, you can get help as soon as you notice any of these types of abuse, no matter how minor they may seem:
- Intimidation
- Destroying property
- Physical assault
- Verbal insults
- Social isolation
- Forced sex
- Harming pets
- Financial, physical, or emotional control
- Coercion to have sex, drink, or take drugs
Domestic violence can happen to anyone, regardless of their age, gender, or social standing. There’s also a complex relationship between substance use and domestic violence.1 These 2 issues often go hand in hand, and each one makes the other more likely.
Both perpetrators and survivors of abuse have high rates of addiction.2
The Impact of Addiction on Domestic Violence
Addiction is common among perpetrators of domestic violence.3 25-50% of intimate partner abusers have substance use disorders. And as an abuser’s addiction grows more severe, both the frequency and severity of their abuse increases.4
It’s important to note that most people experiencing addiction are not violent5 towards others. However, the influence of drugs or alcohol can make people with violent tendencies more likely to act on them.
By definition, being drunk or high changes your brain chemistry.6 As a result, drinking or using drugs can change the way you think, feel, and react to stress. You might be less capable of controlling your anger, making violence more likely. Ongoing drug use increases your risk of violent behavior7 over time.
Social norms can also contribute to higher rates of violence. In some cultures, “I was drunk” is an acceptable excuse for a wide range of negative behavior, from telling secrets to picking fights. When people feel like they can blame their actions on substances, they may drink or use drugs to justify ongoing violence.8 This mindset can also prevent them from getting the help they need.
Women experiencing alcohol or drug addiction are also more likely to become victims of domestic violence.9 However, studies show that this often relates to their partners’ substance abuse issues even more than their own.
Substance use doesn’t cause domestic violence. And blaming violence on a person’s addiction—whether they’re the survivor or the perpetrator—removes the abuser’s responsibility.
Explore Post Traumatic Stress Disorder Treatment Centers
Facts on Substance Abuse and Domestic Violence
Data shows a strong connection between correlate substance use and domestic violence:
- Domestic violence survivors are nearly 6 times more likely to develop alcohol addiction.
- Nearly 50% of women who enter addiction treatment are domestic violence survivors. The rates are much higher for women in opioid addiction treatment.
- When both people in a relationship use substances, their risk of interpersonal violence goes up.
- 39% of incarcerated abusers have a history of alcohol addiction.
- 22% of incarcerated abusers have a history of drug addiction.
- Substance use is involved in up to 80% of child abuse cases.
- Teens and young adults who were abused in childhood have a higher risk of addiction.
- Serious physical violence occurs in 8-13% of all marriages.
- Women who abuse substances are at a higher risk of domestic violence.
How Domestic Violence Can Lead to Addiction
Domestic violence survivors are at a high risk of addiction.12 That’s partly because it’s so common for survivors to self-medicate13 the symptoms of trauma. Survivors are also more likely to experience mental health issues.14 So they may use drugs or alcohol to cope with the symptoms of another diagnosis, like post-traumatic stress disorder (PTSD).
Addiction in Survivors of Intimate Partner Violence
Many people cope with the trauma of intimate partner violence (IPV) by using drugs or alcohol.19 For many survivors, this occasional coping method quickly turns into addiction—especially if you lack other coping strategies. Survivors of IPV also tend to have more severe addiction symptoms.
Physical injuries from IPV can also lead to addiction. For example, it’s common for IPV to result in chronic pain or traumatic brain injury. Both of these conditions increase your risk of addiction. But developing an addiction also increases your risk of experiencing IPV again, and this can quickly become a cycle. Seeking treatment can keep you safe from further violence.
Special Considerations for Men Who Have Survived Domestic Violence
Although most research focuses on women survivors, 25-50% of people who survive IPV each year are men.20 And like women, studies show that male survivors of domestic violence are more likely to develop addiction. But the cultural stigma that male survivors face can be a barrier to treatment and recovery.
Treatment for Addiction and Domestic Violence-Related Trauma
When you’re recovering from abuse and addiction, it’s ideal to find treatment that addresses both at the same time. Studies show that comprehensive treatment is more effective21 than seeking help for trauma and addiction separately.
How Does Comprehensive Treatment Work?
Most rehabs that address both addiction and domestic violence offer trauma-informed care. Trauma affects everyone differently, and its impacts can be surprising. A trauma-informed approach accounts for your unique needs during recovery, even as those needs change.
Recognizing your triggers and respecting your boundaries is a huge part of this. For example, you’ll be able to say “stop” at any point in therapy, and take a break or change the subject. The physical environment will also be conducive to healing with well-lit common areas, no loud noises, and safety features like security personnel at entrances and exits.
Integrated treatment also accounts for the role of trauma in addiction.22 For example, if you’re in cognitive behavioral therapy (CBT), you might learn how to cope with trauma triggers without using drugs or alcohol. These skills can help you navigate long-term recovery from both conditions.
Aftercare Planning for Survivors of Domestic Violence
For survivors, aftercare includes more than ongoing mental health support. While that’s important, it’s just one part of your safety. In most programs, you can start planning for aftercare as soon as you enter treatment.
When you start rehab, your therapist may ask you to sign a no-contact contract,23 where you’ll agree not to communicate with your abuser during treatment. But after rehab, it’s not always that simple. If you have children with them or share assets like a house, the legal system may require some amount of contact.
It’s also common for survivors to be socially isolated24 and have fewer financial resources immediately after an abusive relationship. So as you approach the end of treatment, you’ll work with your therapist to create a concrete safety plan25 for after you leave. That plan might include:
- Intentions around if, when and how you’ll be in contact with your abuser, including information about your legal rights
- A safe place to live
- A new phone number, email address or other contact information your abuser won’t have access to
- A local therapist
- In-person support groups
- Relevant hotlines for social services
- Other community resources
Healing from abuse is a deeply personal process, and every survivor has unique needs. Your provider can help you find the resources you need to achieve your recovery goals.
You can start healing from abuse and addiction in treatment centers around the world. Rehabs that treat trauma will help you plan for a safer, brighter future.
Frequently Asked Questions About Domestic Violence and Addiction
How does substance use affect domestic violence?
Substance use is common among both perpetrators and survivors of domestic violence, and it can increase the risk and severity of violent behavior. Alcohol and drugs change brain chemistry, making it harder to control anger and increasing the likelihood of violence.
How can rehab help with domestic violence and addiction?
Rehabs that specialize in treating both addiction and trauma offer a safe, supportive space where survivors can heal from the trauma of abuse while also addressing their addiction. Treatment often includes individual and group therapy, medical care, and complementary therapies. Rehab can also provide survivors with the skills and tools they need to build a healthy, substance-free life after leaving the program. It’s important to choose a rehab that’s equipped to handle both issues and has experience working with survivors of domestic violence.
-
Center for Substance Abuse Treatment. Substance Abuse Treatment and Domestic Violence. Rockville (MD): Substance Abuse and Mental Health Services Administration (US); 1997. (Treatment Improvement Protocol (TIP) Series, No. 25.) Chapter 1—Effects of Domestic Violence on Substance Abuse Treatment. Available from: https://www.ncbi.nlm.nih.gov/books/NBK64441/
-
Rivera, E. A., Phillips, H., Warshaw, C., Lyon, E., Bland, P. J., Kaewken, O. (2015). An applied research paper on the relationship between intimate partner violence and substance use. Chicago, IL: National Center on Domestic Violence, Trauma & Mental Health.
-
Center for Substance Abuse Treatment. Substance Abuse Treatment and Domestic Violence. Rockville (MD): Substance Abuse and Mental Health Services Administration (US); 1997. (Treatment Improvement Protocol (TIP) Series, No. 25.) Chapter 1—Effects of Domestic Violence on Substance Abuse Treatment. Available from: https://www.ncbi.nlm.nih.gov/books/NBK64441/
-
Violent Substance Abusers in Domestic Violence Treatment | Office of Justice Programs. https://www.ojp.gov/ncjrs/virtual-library/abstracts/violent-substance-abusers-domestic-violence-treatment. Accessed 19 Apr. 2023.
-
Fact Sheet: Substance Abuse and Domestic Violence. Center for Court Innovation, https://www.supremecourt.ohio.gov/docs/JCS/domesticViolence/topics/DVCourts/DVSubstanceAbuse.pdf.
-
Center for Substance Abuse Treatment. Substance Abuse Treatment and Domestic Violence. Rockville (MD): Substance Abuse and Mental Health Services Administration (US); 1997. (Treatment Improvement Protocol (TIP) Series, No. 25.) Chapter 1—Effects of Domestic Violence on Substance Abuse Treatment. Available from: https://www.ncbi.nlm.nih.gov/books/NBK64441/
-
Zhong S, Yu R, Fazel S. Drug Use Disorders and Violence: Associations With Individual Drug Categories. Epidemiol Rev. 2020 Jan 31;42(1):103-116. doi: 10.1093/epirev/mxaa006. PMID: 33005950; PMCID: PMC7879597.
-
Center for Substance Abuse Treatment. Substance Abuse Treatment and Domestic Violence. Rockville (MD): Substance Abuse and Mental Health Services Administration (US); 1997. (Treatment Improvement Protocol (TIP) Series, No. 25.) Chapter 1—Effects of Domestic Violence on Substance Abuse Treatment. Available from: https://www.ncbi.nlm.nih.gov/books/NBK64441/
-
Klein, Andrew. “Practical Implications of Current Domestic Violence Research.” National Institute of Justice. https://www.ojp.gov/pdffiles1/nij/225722.pdf
-
Yu R, Nevado-Holgado AJ, Molero Y, D'Onofrio BM, Larsson H, Howard LM, Fazel S. Mental disorders and intimate partner violence perpetrated by men towards women: A Swedish population-based longitudinal study. PLoS Med. 2019 Dec 17;16(12):e1002995. doi: 10.1371/journal.pmed.1002995. PMID: 31846461; PMCID: PMC6917212.
-
Trevillion K, Oram S, Feder G, Howard LM. Experiences of domestic violence and mental disorders: a systematic review and meta-analysis. PLoS One. 2012;7(12):e51740. doi: 10.1371/journal.pone.0051740. Epub 2012 Dec 26. PMID: 23300562; PMCID: PMC3530507.
-
Center for Substance Abuse Treatment. Substance Abuse Treatment and Domestic Violence. Rockville (MD): Substance Abuse and Mental Health Services Administration (US); 1997. (Treatment Improvement Protocol (TIP) Series, No. 25.) Chapter 1—Effects of Domestic Violence on Substance Abuse Treatment. Available from: https://www.ncbi.nlm.nih.gov/books/NBK64441/
-
Hines DA, Douglas EM. Alcohol and drug abuse in men who sustain intimate partner violence. Aggress Behav. 2012 Jan-Feb;38(1):31-46. doi: 10.1002/ab.20418. Epub 2011 Oct 25. PMID: 22028251; PMCID: PMC3315600.
-
Abuse, Trauma, and Mental Health | Office on Women’s Health. https://www.womenshealth.gov/mental-health/abuse-trauma-and-mental-health. Accessed 19 Apr. 2023.
-
Hines DA, Douglas EM. Alcohol and drug abuse in men who sustain intimate partner violence. Aggress Behav. 2012 Jan-Feb;38(1):31-46. doi: 10.1002/ab.20418. Epub 2011 Oct 25. PMID: 22028251; PMCID: PMC3315600.
-
Adverse Childhood Experiences (ACEs). 6 June 2022, https://www.cdc.gov/violenceprevention/aces/index.html.
-
Fast Facts: Preventing Adverse Childhood Experiences |Violence Prevention|Injury Center|CDC. 14 Apr. 2022, https://www.cdc.gov/violenceprevention/aces/fastfact.html.
-
Mair C, Cunradi CB, Todd M. Adverse childhood experiences and intimate partner violence: testing psychosocial mediational pathways among couples. Ann Epidemiol. 2012 Dec;22(12):832-9. doi: 10.1016/j.annepidem.2012.09.008. Epub 2012 Oct 18. PMID: 23084843; PMCID: PMC3508260.
-
Mehr JB, Bennett ER, Price JL, de Souza NL, Buckman JF, Wilde EA, Tate DF, Marshall AD, Dams-O'Connor K, Esopenko C. Intimate partner violence, substance use, and health comorbidities among women: A narrative review. Front Psychol. 2023 Jan 27;13:1028375. doi: 10.3389/fpsyg.2022.1028375. PMID: 36778165; PMCID: PMC9912846.
-
Hines DA, Douglas EM. Alcohol and drug abuse in men who sustain intimate partner violence. Aggress Behav. 2012 Jan-Feb;38(1):31-46. doi: 10.1002/ab.20418. Epub 2011 Oct 25. PMID: 22028251; PMCID: PMC3315600.
-
James J. Collins ; Donna L. Spencer ; Jeanne A. Snodgrass ; Sara C. Wheeless “Linkage of Domestic Violence and Substance Abuse Services, Final Report.” April 2002. https://www.ojp.gov/pdffiles1/nij/grants/194123.pdf
-
James J. Collins ; Donna L. Spencer ; Jeanne A. Snodgrass ; Sara C. Wheeless “Linkage of Domestic Violence and Substance Abuse Services, Final Report.” April 2002. https://www.ojp.gov/pdffiles1/nij/grants/194123.pdf
-
“Substance Abuse Treatment and Domestic Violence.” Substance Abuse and Mental Health Services Administration Substance Abuse and Mental Health Services Administration, Center for Substance Abuse Treatment. Treatment Improvement Protocol (TIP) Series 25. https://store.samhsa.gov/sites/default/files/SAMHSA_Digital_Download/SMA12-3390_508.pdf
-
Klein, Andrew. “Practical Implications of Current Domestic Violence Research.” National Institute of Justice. https://www.ojp.gov/pdffiles1/nij/225722.pdf
-
“Substance Abuse Treatment and Domestic Violence.” Substance Abuse and Mental Health Services Administration Substance Abuse and Mental Health Services Administration, Center for Substance Abuse Treatment. Treatment Improvement Protocol (TIP) Series 25. https://store.samhsa.gov/sites/default/files/SAMHSA_Digital_Download/SMA12-3390_508.pdf
Our Promise
How Is Recovery.com Different?
We believe everyone deserves access to accurate, unbiased information about mental health and recovery. That’s why we have a comprehensive set of treatment providers and don't charge for inclusion. Any center that meets our criteria can list for free. We do not and have never accepted fees for referring someone to a particular center. Providers who advertise with us must be verified by our Research Team and we clearly mark their status as advertisers.
Our goal is to help you choose the best path for your recovery. That begins with information you can trust.






