Psychedelic Therapy: A New Treatment for PTSD



Sarah holds a B.A. in Psychology from the University of Wisconsin-Madison where she was part of a psycho-social research lab. She is the Content Manager and Editor at Recovery.com, creating informational video resources on behavioral health.

Dr. Mala, is the Chief Clinical Officer at Recovery.com, where she develops impartial and informative resources for people seeking addiction and mental health treatment.




Sarah holds a B.A. in Psychology from the University of Wisconsin-Madison where she was part of a psycho-social research lab. She is the Content Manager and Editor at Recovery.com, creating informational video resources on behavioral health.

Dr. Mala, is the Chief Clinical Officer at Recovery.com, where she develops impartial and informative resources for people seeking addiction and mental health treatment.
Psychedelic therapy has been gaining traction and creating a reputable name for itself in the recovery community. The curiosity around psychedelic treatment for mental health began in the 1950s (although medicinal psychedelic use originates back hundreds of years) when LSD showed initial therapeutic promise in human trials. In the mid 1960s, a legislative ban was placed on this research.1
Fast forward to 1994, psychedelics such as psilocybin were approved once again for research in the United States. Today, the Multidisciplinary Association for Psychedelic Studies (MAPS) serves as the foundation for human neuroimaging, psychology, and psychopharmacology studies with psychedelics.2
Psychedelic therapy is becoming more and more common among providers, specifically for disorders like post-traumatic stress disorder (PTSD), depression, and anxiety. This new age approach to healing offers patients a plethora of benefits, especially for those who do not resonate with traditional therapies.
What Is Psychedelic Therapy?
Psychedelic therapy uses psychedelic substances such as psilocybin (naturally occurring in magic mushrooms), MDMA (commonly known as ecstasy), and LSD within a controlled therapeutic setting. Their therapeutic use can facilitate mental health recovery and personal growth.
Psychedelics alter your state of consciousness, usually producing positive changes in perception, thought patterns, emotions, and a sense of interconnectedness.3 Each psychedelic is slightly different in how it affects your mind and body, but research has shown a positive association between psychedelic use and mental health.1
Through psychedelic treatment, qualified professionals can reach deeper into patients’ thoughts, feelings, and consciousness. This allows therapy sessions to reveal challenges that may be harder to process in traditional therapy. It’s unlocking new ways of healing.
How Psychedelics Affect the Brain
When you’re using psychedelic substances, your brain functions differently. You can visually see this on an EEG or CAT scan showing the difference between normal brain functioning and a brain on psychedelics.
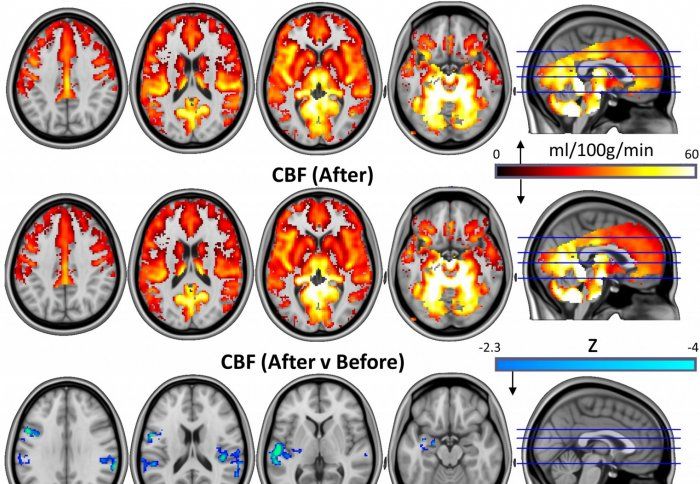
This image shows an increase of brain connectivity and blood flow.4
Psychedelics cause a disruption of electrical synchronicity in the brain.5 This asynchronicity produces an “entropic” state, or an increase in connectivity between brain networks that may not typically communicate with each other. This can lead to a more integrated experience of thoughts, sensations, and emotions. Psychedelics can boost creativity and problem solving through the increased connectivity.6 And they can elevate mood.
Researchers and mental health professionals then use this connectivity to help patients open up about their emotions and process difficult memories and feelings.
Psychedelics for Post-Traumatic Stress Disorder
Psychedelics show great promise to the mental health recovery community. Specifically, psilocybin and MDMA may have positive implications for PTSD recovery.
How Psychedelics Help a Brain with PTSD
Psilocybin
Psilocybin stimulates neurogenesis—the growth and repair of brain cells—particularly in the hippocampus, responsible for memory and emotion.7 Neuron regrowth in this specific brain region allows PTSD patients to reframe and process traumatic memories in a less distressing way.
MDMA
Bessel van der Kolk, one of the top experts on trauma, dove into researching the promising effects of MDMA recovery for patients with severe PTSD.8 Two months after participating in the study, more than 66% of those who were administered MDMA no longer had diagnosable PTSD9.
Why? MDMA can enhance trust, empathy, and communication between the patient and therapist. It reduces fear and anxiety responses while increasing emotional openness. This helps PTSD patients to revisit and process traumatic memories in a more controlled and comfortable manner.
Psychedelics as a Whole
Psychedelics bolster trauma processing by temporarily reducing activity in the Default Mode Network (DMN), responsible for rumination and mind wandering.10 These thought processes are commonly associated with mental health conditions like PTSD. Decreasing activity in this region prevents painful thoughts from coming up when talking about traumatic experiences.
Psychedelics also improve overall brain functioning. Mental health conditions often result in neuron atrophy, or neuron destruction, in the prefrontal cortex.11 Studies have shown that psychedelics can boost neuroplasticity in the brain, meaning they can help the expansion of these neural networks. Rebuilding damage in the brain leaves room for mental health growth and learning new coping skills.
What Does This Mean for PTSD Patients?
Psychedelic therapy offers PTSD patients a new way to heal. With a qualified therapist, you may be able to explore areas of yourself you have hidden due to trauma.
The increased emotional intensity that psychedelics generate can help patients confront and process repressed emotions, traumas, and unresolved issues, potentially leading to therapeutic breakthroughs.
Many patients also gain new insights and ideas while on psychedelics, which is particularly helpful when exploring personal challenges or problem solving.
Psychedelics can enhance emotional regulation and resilience. MDMA in particular has been associated with increased empathy, trust, and emotional openness, which can help patients better manage intense emotions related to their trauma.
The Treatment Process
If you’re interested in adding psychedelic therapy to your treatment plan, you can expect your sessions to be monitored by trained professionals in a safe environment. Before the session, the therapist will conduct an extensive assessment to ensure that you are a suitable candidate for psychedelic therapy. They should also try to identify any potential risks.
At your session, you’ll relax in a comfortable position, typically lying down with eye shades and headphones to minimize external distractions and enhance introspection. The carefully measured psychedelic dosage aligns with your body weight and previous experiences.
During the psychedelic experience, you’ll do some emotional exploration. Your therapist will help guide your thoughts, emotions, memories, and sensations. You’ll talk about specific traumatic experiences you’ve experienced. The therapist may ask open-ended questions, help you through challenging emotions, or offer reassurance.
After the session is complete, your therapist will stay with you and ensure you’re comfortable until you stop feeling the psychedelic effects.
You and your therapist will integrate the lessons and insights you’re learning into the rest of your treatment plan and daily life. This may involve setting intentions for future growth and healing.
Finding Qualified Psychedelic Therapy
Finding a qualified clinic for your psychedelic therapy experience is crucial to guarantee you have safe and effective sessions.
First, research clinics in your area (and make sure this therapy is legal in your state/country). If you don’t know where to start, ask your primary care doctor for recommendations. The treatment team should have a background in psychology, counseling, psychiatry, or a related field. The therapists should also have additional training in psychedelic-assisted therapy. Make sure they have experience administering this treatment.
Then, schedule a consultation with the practice. You can ask questions like
- What safety guidelines do you have in place?
- What are your therapists’ qualifications?
- Can sessions be tailored to my specific needs?
- How long will my sessions last? How many sessions will I have?
- How much do your sessions cost? Will insurance cover them?
If you feel comfortable after talking to the clinic, then you may be on your way to beginning your psychedelic therapy sessions.
Benefits and Risks
Psychedelic therapy shows the potential to be a major player in PTSD recovery; however, this is an emerging form of therapy. It’s always best to check with your doctor to see if you’re a fit. Before you start treatment, a psychedelic therapy clinic should complete a comprehensive physical and mental health assessment.
Psychedelic therapy benefits patients not only by improving mental health but it’s also a great approach for people with treatment-resistant PTSD.12 Psychedelic effects can break through hard to reach areas in the brain by promoting deep self-reflection and insight.
Psychedelics don’t cause addiction or withdrawal, making this therapy a viable option for PTSD patients with co-occurring substance use disorders.5
However, the psychedelic field is still growing. There is still a lack of long-term clinical trials to fully understand the benefits and risks of psychedelic therapy. And without proper supervision, psychedelics can produce intense and unpredictable experiences. They can also trigger psychotic episodes in patients vulnerable to psychosis, so thorough screening is essential.
Receiving treatment at qualified practices that supervise sessions and provide a clean, safe space will likely guarantee that you have a positive session.
Legality and Ethics
While some regions have decriminalized psychedelics or keep them regulated for medical use, psychedelics are illegal in many parts of the world; however, many areas are reevaluating their potential therapeutic applications. For example, the United States Food and Drug Administration (FDA) has granted “breakthrough therapy” status to some psychedelic compounds, which expedites their development as treatment for specific mental health conditions such as PTSD and depression.13
Psychedelic therapy is ethical for patients so long as they give informed consent and are aware of the potential risks. They should have proper screening and risk assessment to identify if they’re at greater risk of adverse reactions, such as a personal or family history of mental illness or certain medical conditions. And before the session, the therapist should explain the psychedelic experience, so the patient knows what to expect.
The Future of Psychedelic Therapy
The movement behind therapeutic psychedelic use will likely continue growing. Expanding research explores the potential of psychedelics in treating a broader range of mental health conditions outside of PTSD, including addiction, eating disorders, and neurodegenerative conditions like Alzheimer’s disease. Additionally, the FDA and other regulatory agencies are actively reviewing clinical trials using psychedelics, so more approvals for medical psychedelic treatments may come. From there, psychedelic therapy is likely to become more integrated into mainstream mental health care.
While the road ahead is not linear, psychedelic therapy may become a staple in healthcare. So long as this therapy has continued research and education, and responsible use, it will continue to make a difference in people’s lives.
Discover a Path to Healing
From intensive individual therapy programs to 24/7 structured support, the right solution is out there. Explore options for wellness-focused mental health treatment, trauma treatment centers, and more to find a safe space to heal. Find a mental health facility today and begin your journey toward stability and peace.
-
Carhart-Harris, R. L., & Goodwin, G. M. (2017). The therapeutic potential of psychedelic drugs: Past, present, and future. Neuropsychopharmacology, 42(11), 2105–2113. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5603818/
-
Maps. Org—Support psychedelic science. (n.d.). Multidisciplinary Association for Psychedelic Studies - MAPS. Retrieved October 11, 2023, from https://maps.org/
-
Earleywine, M. (2005). Mind-altering drugs: The science of subjective experience. Oxford University Press. https://books.google.com/books?hl=en&lr=&id=NAPiBwAAQBAJ&oi=fnd&pg=PT36&dq=psychedelics+alter+your+consciousness&ots=rBf7FZNopw&sig=zlkB8A4ISzTLz2wogztzW1Ji20g#v=onepage&q&f=false
-
Magic mushrooms may “reset” the brains of depressed patients | Imperial News | Imperial College London. (2017, October 13). Imperial News. https://www.imperial.ac.uk/news/182410/magic-mushrooms-reset-brains-depressed-patients/
-
Nutt, D., Spriggs, M., & Erritzoe, D. (2023). Psychedelics therapeutics: What we know, what we think, and what we need to research. Neuropharmacology, 223, 109257. https://www.sciencedirect.com/science/article/pii/S0028390822003161
-
Wießner, I., Falchi, M., Maia, L. O., Daldegan-Bueno, D., Palhano-Fontes, F., Mason, N. L., Ramaekers, J. G., Gross, M. E., Schooler, J. W., Feilding, A., Ribeiro, S., Araujo, D. B., & Tófoli, L. F. (2022). LSD and creativity: Increased novelty and symbolic thinking, decreased utility and convergent thinking. Journal of Psychopharmacology (Oxford, England), 36(3), 348–359. https://pubmed.ncbi.nlm.nih.gov/35105186/
-
Post-traumatic stress disorder treatment with psychedelic drugs. (n.d.). NYU Langone Health. Retrieved October 11, 2023, from https://med.nyu.edu/departments-institutes/population-health/divisions-sections-centers/medical-ethics/education/high-school-bioethics-project/learning-scenarios/ptsd-treatment-psychedelics
-
Best-selling trauma research author. (n.d.). Bessel van Der Kolk, MD. Retrieved October 11, 2023, from https://www.besselvanderkolk.com/
-
Molly, psychedelic drug, shows great promise as mental health…. (n.d.). Bessel van Der Kolk, MD. Retrieved October 11, 2023
-
Gattuso, J. J., Perkins, D., Ruffell, S., Lawrence, A. J., Hoyer, D., Jacobson, L. H., Timmermann, C., Castle, D., Rossell, S. L., Downey, L. A., Pagni, B. A., Galvão-Coelho, N. L., Nutt, D., & Sarris, J. (2022). Default mode network modulation by psychedelics: A systematic review. International Journal of Neuropsychopharmacology, 26(3), 155–188. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10032309/
-
Ly, C., Greb, A. C., Cameron, L. P., Wong, J. M., Barragan, E. V., Wilson, P. C., Burbach, K. F., Zarandi, S. S., Sood, A., Paddy, M. R., Duim, W. C., Dennis, M. Y., McAllister, A. K., Ori-McKenney, K. M., Gray, J. A., & Olson, D. E. (2018). Psychedelics promote structural and functional neural plasticity. Cell Reports, 23(11), 3170–3182. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6082376/
-
Mohamed, A., Touheed, S., Ahmed, M., Hor, M., & Fatima, S. (n.d.). The efficacy of psychedelic-assisted therapy in managing post-traumatic stress disorder (Ptsd): A new frontier? Cureus, 14(10), e30919. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9710723/
-
FDA Grants Breakthrough Therapy Designation for MDMA-Assisted Therapy for PTSD, Agrees on Special Protocol Assessment for Phase 3 Trials. (2017, August 26). Multidisciplinary Association for Psychedelic Studies. https://maps.org/news/media/press-release-fda-grants-breakthrough-therapy-designation-for-mdma-assisted-psychotherapy-for-ptsd-agrees-on-special-protocol-assessment-for-phase-3-trials/
Our Promise
How Is Recovery.com Different?
We believe everyone deserves access to accurate, unbiased information about mental health and recovery. That’s why we have a comprehensive set of treatment providers and don't charge for inclusion. Any center that meets our criteria can list for free. We do not and have never accepted fees for referring someone to a particular center. Providers who advertise with us must be verified by our Research Team and we clearly mark their status as advertisers.
Our goal is to help you choose the best path for your recovery. That begins with information you can trust.









