Ketamine Withdrawal: What to Expect in Detox and Recovery



Hannah is a holistic wellness writer who explores post-traumatic growth and the mind-body connection through her work for various health and wellness platforms. She is also a licensed massage therapist who has contributed meditations, essays, and blog posts to apps and websites focused on mental health and fitness.

Dr. Mala, is the Chief Clinical Officer at Recovery.com, where she develops impartial and informative resources for people seeking addiction and mental health treatment.




Hannah is a holistic wellness writer who explores post-traumatic growth and the mind-body connection through her work for various health and wellness platforms. She is also a licensed massage therapist who has contributed meditations, essays, and blog posts to apps and websites focused on mental health and fitness.

Dr. Mala, is the Chief Clinical Officer at Recovery.com, where she develops impartial and informative resources for people seeking addiction and mental health treatment.
Table of Contents
- What Is Ketamine?
- Signs of Ketamine Addiction
- Ketamine Withdrawal Explained
- Ketamine Detox
- Is Medical Supervision Necessary?
- Ketamine’s Therapeutic Benefits vs. The Realities of Addiction
- Treatment Options for Ketamine Addiction
- Tips for Quitting Ketamine
- The Next Step: Connect With a Ketamine Addiction Treatment Specialist
Ketamine started as a medication used for anesthesia, but today it’s also used in therapeutic settings and recreationally. But like many substances that alter brain chemistry, regular ketamine use can lead your body to adapt and depend on it, meaning you might have withdrawal symptoms when you decide to stop.
Whether you’re personally navigating ketamine use, exploring treatment possibilities, or supporting a loved one through their journey to quit, understanding withdrawal can make the path forward clearer. Let’s explore what happens when ketamine leaves your system, how to manage the process safely, and what support options can help ease the transition back to life without it.
What Is Ketamine?
Ketamine is a medication that first appeared in the ’60s as an anesthetic for surgeries.1 It works by blocking certain chemical receptors in your brain, which makes you feel disconnected from pain, negative emotions, and your surroundings. Doctors and medical teams still use ketamine today in hospitals for procedures requiring sedation.
In recent years, doctors started using ketamine to treat certain mental health conditions.2 In controlled medical settings, it can promote healing for people struggling with treatment-resistant depression, severe anxiety, or PTSD.
Some people also use ketamine recreationally for its dissociative effects—a feeling of detachment from reality, visual distortions, and euphoria. On the street, you might hear it called “special K,” “ket,” “kit kat,” or simply “K.”

Ketamine affects your brain by blocking NMDA receptors, which help with memory, learning, and pain perception.3 It also boosts levels of a brain chemical called glutamate and may affect other neurotransmitters like dopamine—one of your brain’s most important “feel-good” chemicals.
When ketamine becomes a regular part of your life, your body adjusts. You’ll likely need more to feel the same effects (tolerance), which can cause you to develop physical and psychological dependence, leaving you with withdrawal symptoms when you stop.
Signs of Ketamine Addiction
Not everyone who uses ketamine will develop a drug addiction, but regular use can make you dependent. Spotting the signs of ketamine addiction early can help you recognize when casual use has crossed into problematic territory.
Physical Signs
When ketamine use has become an addiction, your body might signal problems through:
- Stomach pain or other digestive troubles
- Changes in your appetite
- Coordination problems that weren’t there before
- Speech that sounds slurred or different
- Breathing difficulties
You might notice bladder problems like needing to pee frequently or having pain when you do—a condition sometimes called “K-bladder“ that can become serious if you continue using.4
One report from ITV News highlights the growing crisis of ketamine-related bladder damage among young people in the UK.5 Dan Parker, a 23-year-old former electrician who nearly lost the use of his bladder after just months of daily ketamine use, recalls his experience of ketamine dependence:
I had it all to lose—everything to lose. Family, friends, relationships, my son. Everything else was gone.
Unlike substances that take decades to cause significant organ damage, ketamine can irreversibly harm the bladder in a much shorter timeframe.6

Behavioral Changes
Just like with other types of substance abuse, ketamine can reshape your daily habits and priorities. You might catch yourself:
- Spending more time and money getting ketamine
- Pulling away from family and friends who care about you
- Letting responsibilities slide as ketamine takes priority
- Dropping activities you used to love because ketamine seems more important
- Performing worse at school or at work
Psychological Symptoms
Ketamine can significantly change how your brain functions, affecting your thoughts and emotions.7 You might struggle with:
- Memory gaps or problems
- Feeling confused or foggy
- Trouble focusing on tasks or conversations
- Mood swings that seem to come out of nowhere
- Intense cravings that are hard to ignore
Many people also experience waves of depression and anxiety, especially after a dose of ketamine when the effects start to wear off.
Impact on Daily Life
When ketamine starts taking center stage, things can start to unravel around you. Maybe you continue using even though it’s causing problems with your health, your relationships, or your job. If you’ve tried to cut back or stop but found it surprisingly difficult, that’s actually a common experience—and a sign that recreational drug use may have developed into something more serious.

Ketamine Withdrawal Explained
When ketamine becomes a regular part of your routine, your brain gets used to having it around. Your brain chemistry actually adapts to function with ketamine in your system. When you decide to stop or cut back, your body needs time to reset—which causes withdrawals.
Why Withdrawal Happens
Your brain has a delicate chemical balance. Ketamine affects special receptors that control how you think, feel, and how your body works.8 With ongoing use, these receptors become less responsive, and your brain produces different levels of natural chemicals to maintain equilibrium. When you suddenly remove ketamine from this equation, things get out of balance until your brain can rebuild its natural systems. This adjustment period is what we call withdrawal.

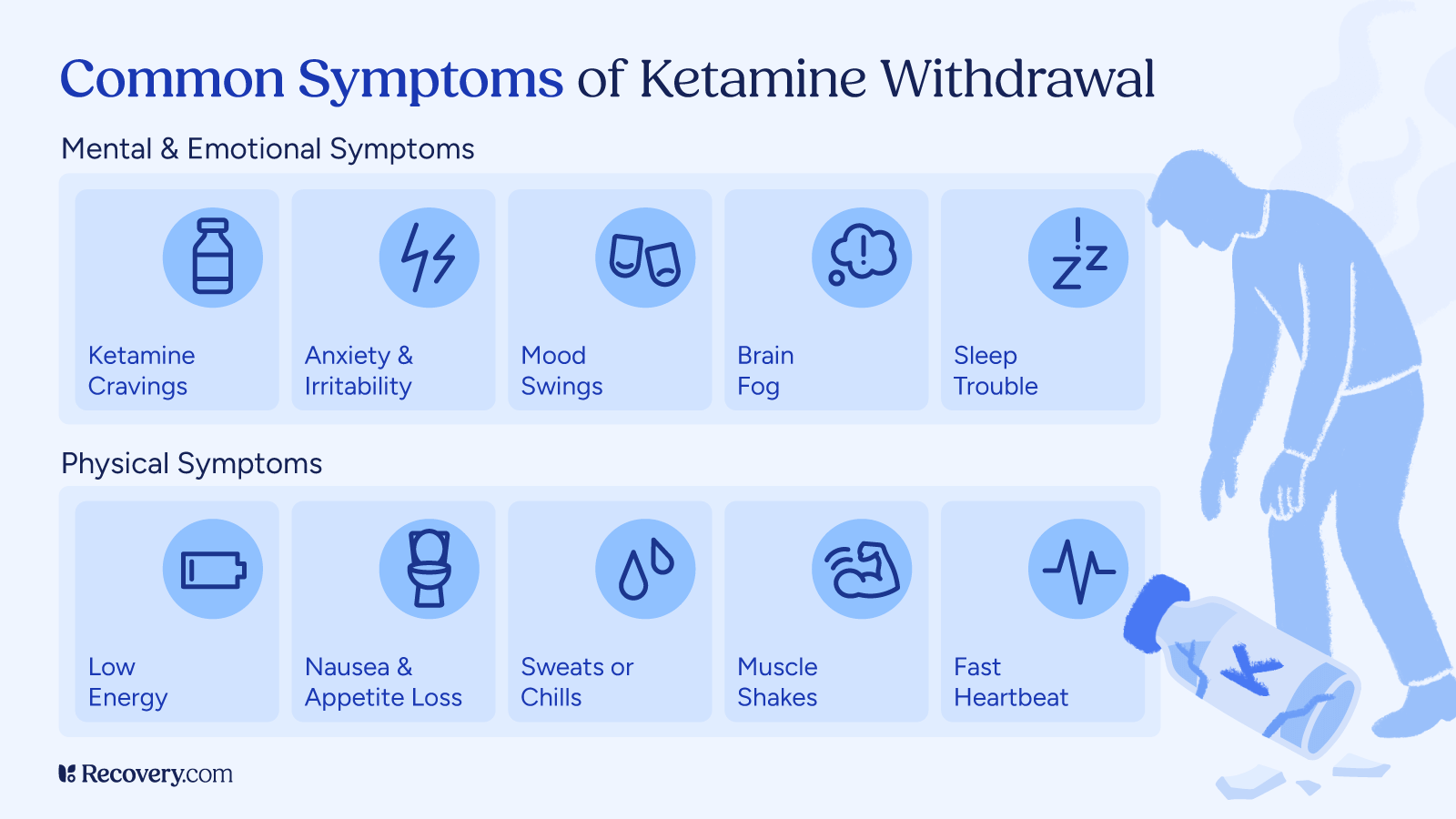
Common Symptoms
While ketamine withdrawal symptoms aren’t typically dangerous, it can certainly be uncomfortable.1 You might experience:
- Strong urges to use ketamine again
- Feeling anxious, restless, or easily irritated
- Waves of depression or mood swings that come and go
- Trouble sleeping or unusual dreams
- Feeling drained of energy
- Foggy thinking and memory blips
- Increased heart rate or higher blood pressure
- Unexpected sweating or chills
- Loss of appetite
- Confusion or feeling disconnected from reality
Some people find that the mental and emotional aspects of ketamine withdrawal hit harder than the physical symptoms.9 Feeling down and fighting those persistent cravings can be especially challenging.
Acute Cases
While ketamine withdrawal isn’t typically life-threatening like alcohol or benzodiazepine withdrawal, some people do experience more severe reactions. Research in the American Journal of Psychiatry highlights cases where people felt extreme agitation and intense mood swings when they stopped taking ketamine cold turkey. In one case, a person who had been taking large amounts of ketamine regularly became highly distressed—hitting walls, yelling, and behaving erratically until he received proper medical help.10
Medical professionals are still working to understand these more intense withdrawal experiences, and there’s no clear definition of what “typical” ketamine withdrawal looks like. For those who use heavily and frequently, symptoms can become acute enough to seriously disrupt daily life. This is why it’s safest to quit ketamine with professional guidance, especially if you’ve been using ketamine regularly for a long time.
Ketamine Withdrawal Timeline
Everyone’s body responds differently to withdrawal, but research shows that ketamine withdrawals can kick in just 24 hours after the last dose.11 Physical withdrawals are usually short-term, but some psychological symptoms—like cravings, mood fluctuations, and sleep troubles—might stick around for longer.
For some people, withdrawal symptoms last longer than expected. Learn more about this extended recovery process and how to navigate it in our guide to post-acute withdrawal syndrome (PAWS).

Factors That Affect Severity
How intense your withdrawal experience feels depends on several personal factors:
- How long you used ketamine
- Your typical dose and how often you’ve been using
- Whether you use other substances alongside ketamine
- Your overall physical and mental well-being
- The support system and environment around you
Withdrawals can test your resolve, both physically and mentally—they’re actually one of the main reasons people return to using. But it’s good to keep in mind that withdrawal is temporary, and with the right support in your corner, you absolutely can make it through this challenging phase of recovery.
Ketamine Detox
While ketamine addiction is certainly treated in professional settings, the concept of “detoxification” for ketamine differs from substances like alcohol, opioids, or benzodiazepines. Unlike those substances, ketamine doesn’t typically cause severe physical withdrawal symptoms that require medical management.12 Most ketamine users don’t need the same kind of monitored detox process that’s necessary for substances that cause more dangerous withdrawals.
When you get treatment for ketamine addiction, the process usually focuses more on:
- Psychological support to manage cravings and mood changes
- Therapy to address underlying causes of your addiction
- Developing coping skills and relapse prevention strategies
- Treatment for any co-occurring mental health conditions
For people who have been using ketamine heavily or in combination with other substances, a more structured environment during the early days of abstinence can still be very beneficial for monitoring mood, providing support, and ensuring a successful transition to your treatment program.
Is Medical Supervision Necessary?
While ketamine withdrawal isn’t typically severe or physically dangerous, professional support during this time can still be invaluable. Treatment providers can help manage psychological issues like depression and cravings, address any co-occurring mental health concerns, and provide structure and accountability to prevent relapse.
For many people, having this support significantly increases their chances of staying on track toward long-term recovery, especially if they’ve used ketamine heavily or for an extended time.
Ketamine’s Therapeutic Benefits vs. The Realities of Addiction
While ketamine shows promising therapeutic benefits for depression and PTSD in clinical settings, we shouldn’t overlook its potential for addiction. Saturn, who has used ketamine extensively over the years, shares an honest perspective:13
“We all have tendencies to get addicted to things pretty easily, especially if you have a lot of traumas and stuff you’ve been through… Basically, if you use illegal drugs and have self-discipline and you do use them as a tool instead of partying, it could help some people. But some drugs some people shouldn’t be taking. We’re all different… I’ve learned that if you do too much of anything, it’s really bad for you.”
His view reminds us that what works as medicine for one person might become problematic for another. Many people who initially try ketamine for its mood-lifting side effects don’t anticipate developing a substance use disorder. He recalls what a close friend went through:
“One of my best friends was stuck on [ketamine] and he was about to have a kid and he had to get off of it before he had a kid and he was struggling really hard. Him and his wife… they had to get help, they couldn’t do it on their own. So yeah, it can be heavily addictive.”
These experiences remind us that while medical ketamine treatments are carefully controlled, recreational use of ketamine carries real risks of developing dependence that often requires professional help to overcome.
Benefits of Quitting Ketamine
Ketamine can take a serious toll on both your mind and body. Even small amounts may cause numbness, confusion, or hallucinations, along with spikes in blood pressure, heart rate, and temperature. Higher doses can lead to more severe consequences.
Quitting ketamine can have wide-ranging benefits, including:
- Better physical health: Long-term use can damage the bladder, kidneys, and digestive system. Stopping ketamine gives your body a chance to heal and helps prevent further harm.
- Improved mental well-being: Ketamine can affect memory, focus, and mood, sometimes leading to depression or anxiety. Quitting allows space for your brain and emotions to recover.
- Healthier relationships: Substance use often strains connections with loved ones. Giving up ketamine opens the door to rebuilding trust and repairing those bonds.
- Stronger daily functioning: Ketamine can interfere with school, work, and responsibilities. Sobriety can bring back clarity, motivation, and balance to your everyday life.
The decision to quit isn’t easy, but recovery is possible. With the right treatment and support, you can start healing and move toward a healthier, more fulfilling life.
Treatment Options for Ketamine Addiction
The support you choose for your recovery journey can make all the difference in your long-term success.
Residential Rehab
Many people benefit from inpatient rehab programs where you live at a treatment facility for 30-90 days. These programs offer structure, daily therapy, and a recovery-focused environment away from triggers and temptations.
Outpatient Therapeutic Approaches
In rehab, your care team will create a treatment plan for you that includes a combination of therapies such as:
- Cognitive behavioral therapy (CBT) helps you identify and change thought patterns that lead to ketamine abuse
- Group therapy connects you with others facing similar challenges
- Motivational enhancement therapy (MET) strengthens your internal drive to maintain your recovery
Support Groups
Joining groups likeNarcotics Anonymous orSMART Recovery provides ongoing encouragement and accountability when formal treatment ends.
Harm Reduction Strategies
If total abstinence doesn’t feel achievable right now, harm reduction strategies can help you use more safely:
- Using less frequently or in smaller amounts
- Avoiding mixing ketamine with other substances
- Having a trusted friend around when using
- Learning about safer administration methods
- Staying hydrated and keeping an eye on your physical health
The Importance of Strong Social Support
In addiction recovery, healthy social support makes all the difference. Supportive friends, family members, or professionals can encourage you when cravings hit hard or when you’re feeling low. Remember that asking for help isn’t a burden—it’s actually a sign of strength and commitment to your recovery.
Aftercare
Aftercare is the stage of recovery where you transition from treatment back into everyday life. It’s an important step as relapse risk is highest during early recovery, so ongoing support can make a big difference.
Aftercare may include:
- Outpatient treatment: Many people continue with outpatient care after completing an inpatient or residential program. This ongoing support helps you stay accountable and receive therapy or check-ins while adjusting to more independence.
- Counseling: Meeting regularly with a therapist (often once a week) can help you work through challenges, maintain progress, and strengthen coping skills as you navigate life after treatment.
- Sober living homes: These structured living environments provide a safe, substance-free place to rebuild your life. Residents agree to stay sober, attend recovery meetings, and follow house rules while working or going to school.
- 12-step programs: Groups like Alcoholics Anonymous (AA) and Narcotics Anonymous (NA) offer a spiritual, community-based approach to recovery. Members attend meetings, find sponsors, and work through the 12 steps together.
- Other support groups: Options like SMART Recovery, Women for Sobriety, LifeRing Secular Recovery, and Secular Organizations for Sobriety (SOS) provide free, peer-led support without a spiritual focus.
Tips for Quitting Ketamine
Quitting ketamine isn’t easy, but it’s possible with the right mindset, plan, and support. Here are some strategies that can help, especially during early recovery:
- Weigh the pros and cons: Make a list of the benefits and drawbacks of both using and quitting ketamine. Focus on the positives of quitting (such as better health, clearer thinking, stronger relationships) and keep that list somewhere visible as a reminder of why you’re making this change.
- Know your triggers: Think about what situations, people, emotions, or environments make you want to use. Understanding your triggers is the first step to learning how to manage or avoid them.
- Create a relapse prevention plan: Once you know your triggers, come up with specific ways to handle them. Some can be avoided (like certain social situations), while others (like stress) require healthy coping skills like deep breathing, exercise, or journaling.
- Prioritize self-care: Taking care of your physical and emotional health can reduce stress, anxiety, and depression, which helps lower your risk of relapse. Try to include activities like regular exercise, meditation, time outdoors, and quality sleep in your routine.
The Next Step: Connect With a Ketamine Addiction Treatment Specialist
Taking steps toward recovery from ketamine use shows incredible courage! Whether you’re just starting to question your relationship with ketamine or you�’re ready to start treatment, support is available every step of the way.
Ready to explore your options? Our treatment finder can connect you with ketamine addiction treatment centers that match your specific needs. These centers offer specialized support to help you navigate withdrawal, develop coping skills, and build a fulfilling life beyond ketamine use—because you deserve the chance to reclaim your health and well-being.
Sources
- Ketamine - an Overview | ScienceDirect Topics. https://www.sciencedirect.com/topics/neuroscience/ketamine. Accessed 11 Apr. 2025.
- MD, Peter Grinspoon. “Ketamine for Treatment-Resistant Depression: When and Where Is It Safe?” Harvard Health, 9 Aug. 2022, https://www.health.harvard.edu/resources/ketamine-for-treatment-resistant-depression-when-and-where-is-it-safe-202208092797.
- Li L, Vlisides PE. Ketamine: 50 Years of Modulating the Mind. Front Hum Neurosci. 2016 Nov 29;10:612. doi: 10.3389/fnhum.2016.00612. PMID: 27965560; PMCID: PMC5126726.
- Leaver, Rachel. Ketamine Bladders: What Community Nurses Should Know. | EBSCOhost. 1 Oct. 2019, https://openurl.ebsco.com/contentitem/gcd:139432648?sid=ebsco:plink:crawler&id=ebsco:gcd:139432648.
- ITV News. (2023, October 9). 'I lost everything': Inside Britain's 'worrying' ketamine problem [Video]. YouTube. https://www.youtube.com/watch?v=ocuulBxy5tg
- Srirangam S, Mercer J. Ketamine bladder syndrome: an important differential diagnosis when assessing a patient with persistent lower urinary tract symptoms. BMJ Case Rep. 2012 Sep 30;2012:bcr2012006447. doi: 10.1136/bcr-2012-006447. PMID: 23035160; PMCID: PMC4544340.
- Shea, C. D. (2023, December 4). New study maps ketamine's effects on brain. Columbia News. https://news.columbia.edu/news/new-study-maps-ketamines-effects-brain
- Galvanho, Jefferson P., et al. “Profiling of Behavioral Effects Evoked by Ketamine and the Role of 5HT2 and D2 Receptors in Ketamine-Induced Locomotor Sensitization in Mice.” Progress in Neuro-Psychopharmacology and Biological Psychiatry, vol. 97, Mar. 2020, p. 109775. ScienceDirect, https://doi.org/10.1016/j.pnpbp.2019.109775.
- Healthdirect Australia. Ketamine. 21 Nov. 2024, https://www.healthdirect.gov.au/ketamine.
- Roxas, Nichole, et al. “A Potential Case of Acute Ketamine Withdrawal: Clinical Implications for the Treatment of Refractory Depression.” American Journal of Psychiatry, vol. 178, no. 7, July 2021, pp. 588–91. DOI.org (Crossref), https://doi.org/10.1176/appi.ajp.2020.20101480.
- Roxas, Nichole, et al. “A Potential Case of Acute Ketamine Withdrawal: Clinical Implications for the Treatment of Refractory Depression.” American Journal of Psychiatry, vol. 178, no. 7, July 2021, pp. 588–91. DOI.org (Crossref), https://doi.org/10.1176/appi.ajp.2020.20101480.
- Center for Substance Abuse Treatment. (2006). Detoxification and substance abuse treatment (Treatment Improvement Protocol Series No. 45; HHS Publication No. SMA 15-4131). U.S. Department of Health and Human Services, Substance Abuse and Mental Health Services Administration. https://library.samhsa.gov/sites/default/files/sma15-4131.pdf
- VICE News. (2023, October 5). How ketamine is being used to treat depression [Video]. YouTube. https://www.youtube.com/watch?v=-Z6FQXZcgKY
FAQs
-
Ketamine - an overview. ScienceDirect Topics: Neuroscience. Elsevier. https://www.sciencedirect.com/topics/neuroscience/ketamine
-
MD, Peter Grinspoon. “Ketamine for Treatment-Resistant Depression: When and Where Is It Safe?” Harvard Health, 9 Aug. 2022. https://www.health.harvard.edu/resources/ketamine-for-treatment-resistant-depression-when-and-where-is-it-safe-202208092797
-
Li L, Vlisides PE. Ketamine: 50 Years of Modulating the Mind. Front Hum Neurosci. 2016 Nov 29;10:612. doi: 10.3389/fnhum.2016.00612. PMID: 27965560; PMCID: PMC5126726. https://pmc.ncbi.nlm.nih.gov/articles/PMC5126726/
-
Leaver, Rachel. Ketamine Bladders: What Community Nurses Should Know. | EBSCOhost. 1 Oct. 2019, https://openurl.ebsco.com/contentitem/gcd:139432648?sid=ebsco:plink:crawler&id=ebsco:gcd:139432648. https://openurl.ebsco.com/EPDB%3Agcd%3A9%3A33455305/detailv2?sid=ebsco%3Aplink%3Ascholar&id=ebsco%3Agcd%3A139432648&crl=c&link_origin=scholar.google.com
-
ITV News. (2023, October 9). 'I lost everything': Inside Britain's 'worrying' ketamine problem [Video]. YouTube. https://www.youtube.com/watch?v=ocuulBxy5tg
-
Srirangam S, Mercer J. Ketamine bladder syndrome: an important differential diagnosis when assessing a patient with persistent lower urinary tract symptoms. BMJ Case Rep. 2012 Sep 30;2012:bcr2012006447. doi: 10.1136/bcr-2012-006447. PMID: 23035160; PMCID: PMC4544340. https://pmc.ncbi.nlm.nih.gov/articles/PMC4544340/
-
Shea, C. D. (2023, December 4). New study maps ketamine's effects on brain. Columbia News. https://news.columbia.edu/news/new-study-maps-ketamines-effects-brain
-
Galvanho, Jefferson P., et al. “Profiling of Behavioral Effects Evoked by Ketamine and the Role of 5HT2 and D2 Receptors in Ketamine-Induced Locomotor Sensitization in Mice.” Progress in Neuro-Psychopharmacology and Biological Psychiatry, vol. 97, Mar. 2020, p. 109775. ScienceDirect, https://doi.org/10.1016/j.pnpbp.2019.109775. https://www.sciencedirect.com/science/article/abs/pii/S0278584619304889
-
Healthdirect Australia. Ketamine. 21 Nov. 2024. https://www.healthdirect.gov.au/ketamine
-
Roxas, Nichole, et al. “A Potential Case of Acute Ketamine Withdrawal: Clinical Implications for the Treatment of Refractory Depression.” American Journal of Psychiatry, vol. 178, no. 7, July 2021, pp. 588–91. DOI.org (Crossref), https://doi.org/10.1176/appi.ajp.2020.20101480. https://psychiatryonline.org/doi/10.1176/appi.ajp.2020.20101480
-
Roxas, Nichole, et al. “A Potential Case of Acute Ketamine Withdrawal: Clinical Implications for the Treatment of Refractory Depression.” American Journal of Psychiatry, vol. 178, no. 7, July 2021, pp. 588–91. DOI.org (Crossref), https://doi.org/10.1176/appi.ajp.2020.20101480. https://psychiatryonline.org/doi/10.1176/appi.ajp.2020.20101480
-
Jones JL, Mateus CF, Malcolm RJ, Brady KT, Back SE. Efficacy of Ketamine in the Treatment of Substance Use Disorders: A Systematic Review. Front Psychiatry. 2018 Jul 24;9:277. doi: 10.3389/fpsyt.2018.00277. PMID: 30140240; PMCID: PMC6094990. https://pmc.ncbi.nlm.nih.gov/articles/PMC6094990/
-
VICE News. (2023, October 5). How ketamine is being used to treat depression [Video]. YouTube. https://www.youtube.com/watch?v=-Z6FQXZcgKY&t=287s
Our Promise
How Is Recovery.com Different?
We believe everyone deserves access to accurate, unbiased information about mental health and recovery. That’s why we have a comprehensive set of treatment providers and don't charge for inclusion. Any center that meets our criteria can list for free. We do not and have never accepted fees for referring someone to a particular center. Providers who advertise with us must be verified by our Research Team and we clearly mark their status as advertisers.
Our goal is to help you choose the best path for your recovery. That begins with information you can trust.









