How Long Does Xanax Stay in Your System? Your Guide to Test Detection



Hannah is a holistic wellness writer who explores post-traumatic growth and the mind-body connection through her work for various health and wellness platforms. She is also a licensed massage therapist who has contributed meditations, essays, and blog posts to apps and websites focused on mental health and fitness.

Dr. Mala, is the Chief Clinical Officer at Recovery.com, where she develops impartial and informative resources for people seeking addiction and mental health treatment.




Hannah is a holistic wellness writer who explores post-traumatic growth and the mind-body connection through her work for various health and wellness platforms. She is also a licensed massage therapist who has contributed meditations, essays, and blog posts to apps and websites focused on mental health and fitness.

Dr. Mala, is the Chief Clinical Officer at Recovery.com, where she develops impartial and informative resources for people seeking addiction and mental health treatment.
When the anxiety-calming effects of Xanax wear off, you might assume the drug has left your system—but testing tells a different story. Xanax (alprazolam) can be detected in your body even if you no longer feel its effects. If you’re starting a new medication, preparing for a drug test, or concerned about interactions with other substances, it’s important to know how long Xanax stays in your system.
Detection times for Xanax can vary depending on a few factors. The type of drug test being used, your personal health, and your usage patterns all affect how long Xanax can be detected. While one person might clear Xanax from their system relatively quickly, another might test positive days later.
We’ll explore exactly how long Xanax is detectable via different testing methods, what affects these timeframes, and what you should know if you’re taking Xanax.
What Is Xanax?
Xanax is the brand name for alprazolam, a type of benzodiazepine. Doctors prescribe Xanax to treat anxiety disorders, panic disorders, and sometimes anxiety caused by depression. Like other benzodiazepines such as Valium (diazepam) and Klonopin (clonazepam), Xanax works by enhancing the calming effects of a naturally occurring brain chemical called gamma-aminobutyric acid (GABA).
When you take Xanax as prescribed, it can effectively reduce feelings of nervousness, tension, and panic attacks. It comes in immediate-release tablets, extended-release tablets, and liquid form. The standard immediate-release Xanax starts working right away, usually within 15-30 minutes, which makes it helpful for managing sudden anxiety episodes.
However, Xanax is also classified as a Schedule IV controlled substance by the DEA.1 This classification exists because Xanax carries a risk for dependence and potential misuse. Your body can develop tolerance to Xanax over time, meaning you might need higher doses to achieve the same effects. This is why doctors typically prescribe Xanax for short-term use—usually no more than 2-4 weeks—to reduce the risk of dependence.
How Xanax Works in the Body
When you take Xanax, your digestive system absorbs the medication into your bloodstream. From there, it travels to your brain where it increases GABA activity, slowing down central nervous system functions and producing a calming effect.2 But what happens to the Xanax molecules after they’ve done their job?
Why does Xanax still show up on drug tests even after the effects of the substance wear off?
How the Body Metabolizes Xanax
Your liver does most of the work to process Xanax. Through a process called metabolism, your liver breaks down Xanax into several metabolites—mainly alpha-hydroxyalprazolam.3 These metabolites eventually leave your body through urine. This entire process, from the moment Xanax enters your body until it exits, is what determines the amount of time it stays in your system.
We know certain medications can significantly affect how quickly someone metabolizes Xanax. What common drug interactions do you find yourself warning patients about most frequently, especially those that might unexpectedly extend detection times?

Xanax Half-Life
An important concept to understand is “half-life,” which refers to the time it takes for your body to eliminate half of the drug from your bloodstream. Xanax has an average half-life of about 11-12 hours in healthy adults.4 This means that 11-12 hours after taking Xanax, roughly half of the drug remains in your system. After another 11-12 hours, half of that remaining amount (or 25% of the original dose) is left, and so on.
Detection Windows for Different Drug Tests
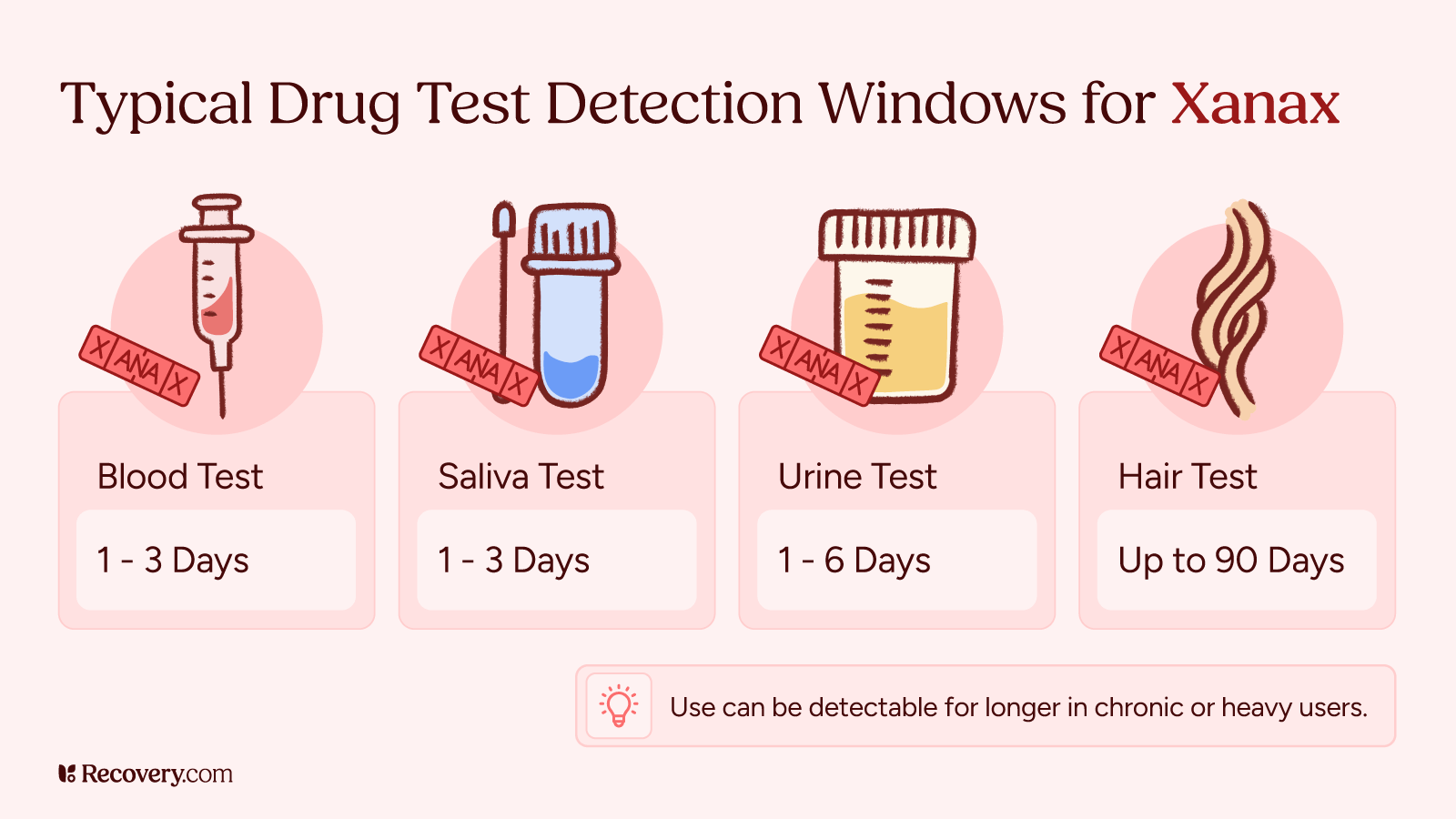
Different drug tests can detect Xanax for different lengths of time after your last dose.
Urine Tests
Urine testing is the most commonly used method to detect Xanax.5 For most people who take Xanax occasionally, it can show up in a urine test for about 1-4 days after the last dose. However, if you’ve been taking Xanax regularly for an extended period, it might be detectable for up to a week or even longer.
When Xanax shows up on a urine test, what the test actually detects are metabolites—the breakdown products of alprazolam. These metabolites have chemical structures that standard drug panels can identify as benzodiazepines. Some tests specifically look for alprazolam metabolites, while others detect a wider range of benzodiazepines.
Blood Tests
Blood tests offer a shorter detection window for Xanax compared to urine tests. Xanax is detectable in blood for about 1-3 days after the last dose.6 Blood testing is less common for routine drug screening but might be used in certain medical or legal situations.
Blood tests aren’t as easy to administer as urine tests, but they provide a more accurate measure of how much Xanax is actively in your system at the time of testing. This makes blood tests useful in emergency situations where doctors need to know exactly what substances are affecting a patient.
Saliva Tests
Saliva tests can detect Xanax for approximately 1-2 days after use.7 These tests are becoming more popular because they’re less invasive and harder to tamper with than urine tests. Collecting a saliva sample is as simple as swabbing the inside of your cheek.
Many people don’t realize that regular Xanax use can build up in body tissues over time. How do you explain this accumulation effect to people who might be concerned about upcoming drug tests or who want to discontinue their medication?

Hair Tests
Hair testing has the longest detection window of all test types. Benzodiazepines can be detected in hair for up to 4 weeks, or even longer in some cases.8 Hair tests work by detecting drug metabolites that enter your bloodstream and then get absorbed into your hair follicles.
Hair tests can detect benzo use over a longer period, but they’re less common for Xanax testing specifically. They’re also less useful for detecting very recent benzo use, as it takes time for the metabolites to appear in hair.
False Positives
It’s worth noting that some substances can trigger false positives for benzodiazepines like Xanax on drug tests.9 These include certain antibiotics, antidepressants, and even some over-the-counter medications like Benadryl (diphenhydramine). If you believe a test has produced a false positive result, you can request confirmation testing, which uses more precise methods to identify specific substances.
What Factors Affect How Long Xanax Stays in Your System?
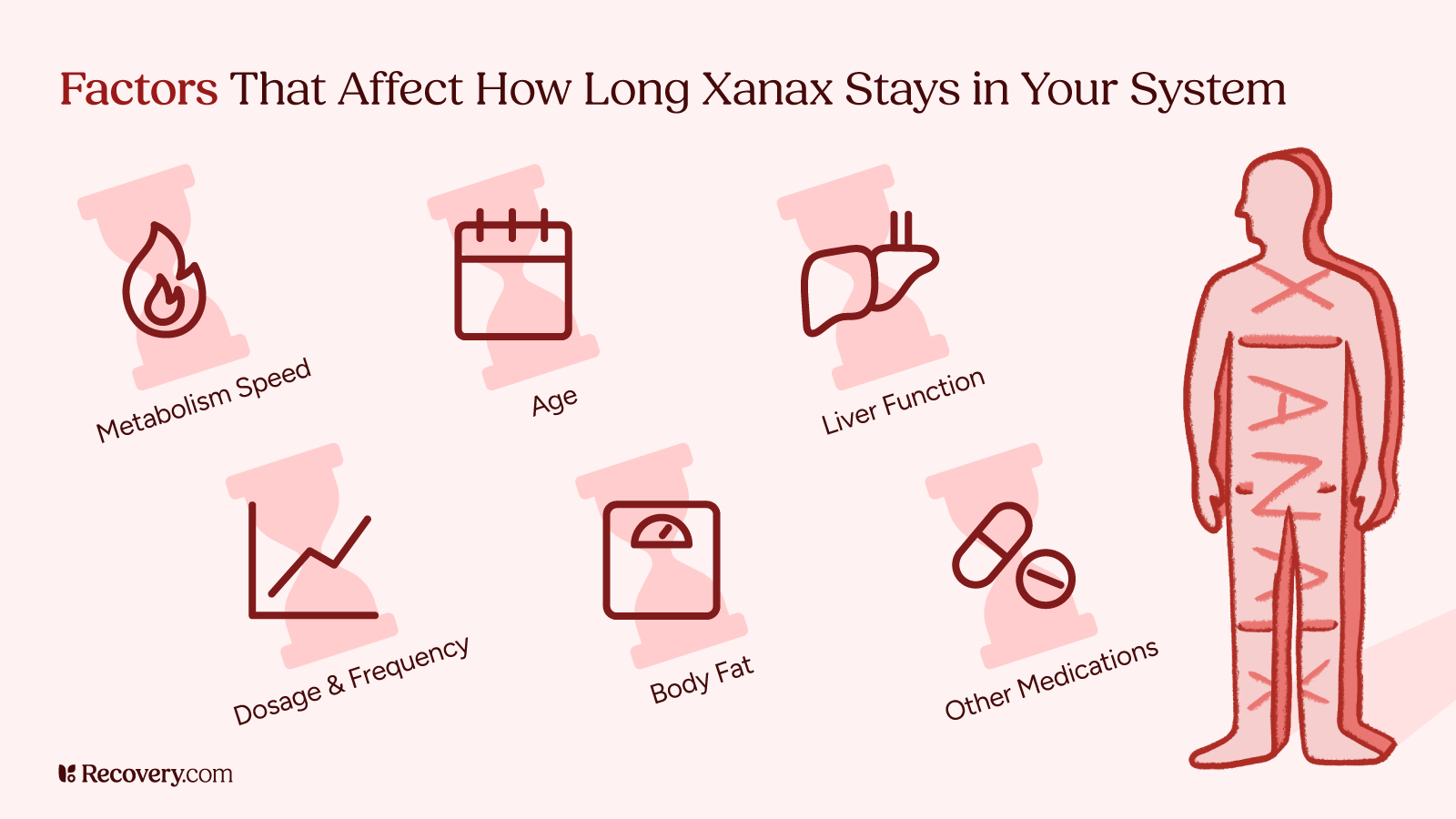
Detection times can vary from person to person because of a few factors that influence how long Xanax stays in your system.
Age and Metabolism
As we age, our metabolism naturally slows down. Older adults often process Xanax more slowly than younger people.10 This means the drug stays in their systems longer and may be detectable for extended periods.
Your metabolic rate—how quickly your body processes substances—also plays a major role. People with faster metabolisms tend to eliminate Xanax more quickly than those with slower metabolisms.
Liver Function
Since your liver is primarily responsible for breaking down benzodiazepines, liver health directly impacts how long Xanax stays in your system.11 People with liver diseases like cirrhosis or hepatitis may take much longer to process and eliminate Xanax. In some cases, doctors might even adjust dosages for patients with liver problems.
Dosage and Frequency of Use
Among the key factors affecting how long Xanax stays in your system, how much and how often you take it are especially important. Your body takes longer to process larger doses. And if you’ve been taking Xanax regularly for weeks or months, it builds up in your system, which takes longer for your body to clear than if you’ve only taken it once or twice.
When you use Xanax regularly, it collects in your body’s fat tissues, creating storage that takes longer to leave your body completely.12 This effect is especially pronounced for people who take high doses over long periods of time.
Body Composition
Your body mass index (BMI) and fat percentage also affect how long Xanax stays in your system. Xanax is lipophilic, meaning it can be stored in fat cells.13 People with higher body fat percentages may end up storing alprazolam in their systems for longer than those with less body fat.
Other Medications
Some medications can affect how quickly you process Xanax.14 For example, certain antifungal medications and antibiotics can impede enzymes in your liver that break down Xanax, causing it to stay in your system longer. On the other hand, some medications might induce these enzymes, making your body clear Xanax faster.
Duration of Xanax Effects vs. Detection Time
Many people don’t realize that Xanax stays in their body long after they stop feeling its effects. This is why you might feel completely normal but still test positive on a drug test.
For regular Xanax tablets, the calming effects typically last up to 6 hours before wearing off. Extended-release Xanax (Xanax XR) works more gradually, with effects lasting up to 12 hours.15 But in both cases, the drug remains in your system much longer than you can feel it.
You need a certain concentration of Xanax in your bloodstream to feel its anxiety-reducing effects. When levels drop below that threshold, the effects wear off. But the drug is still there at lower levels until your body completely processes it, which takes several days. During this time, drug tests can still detect Xanax even though you no longer feel its effects.
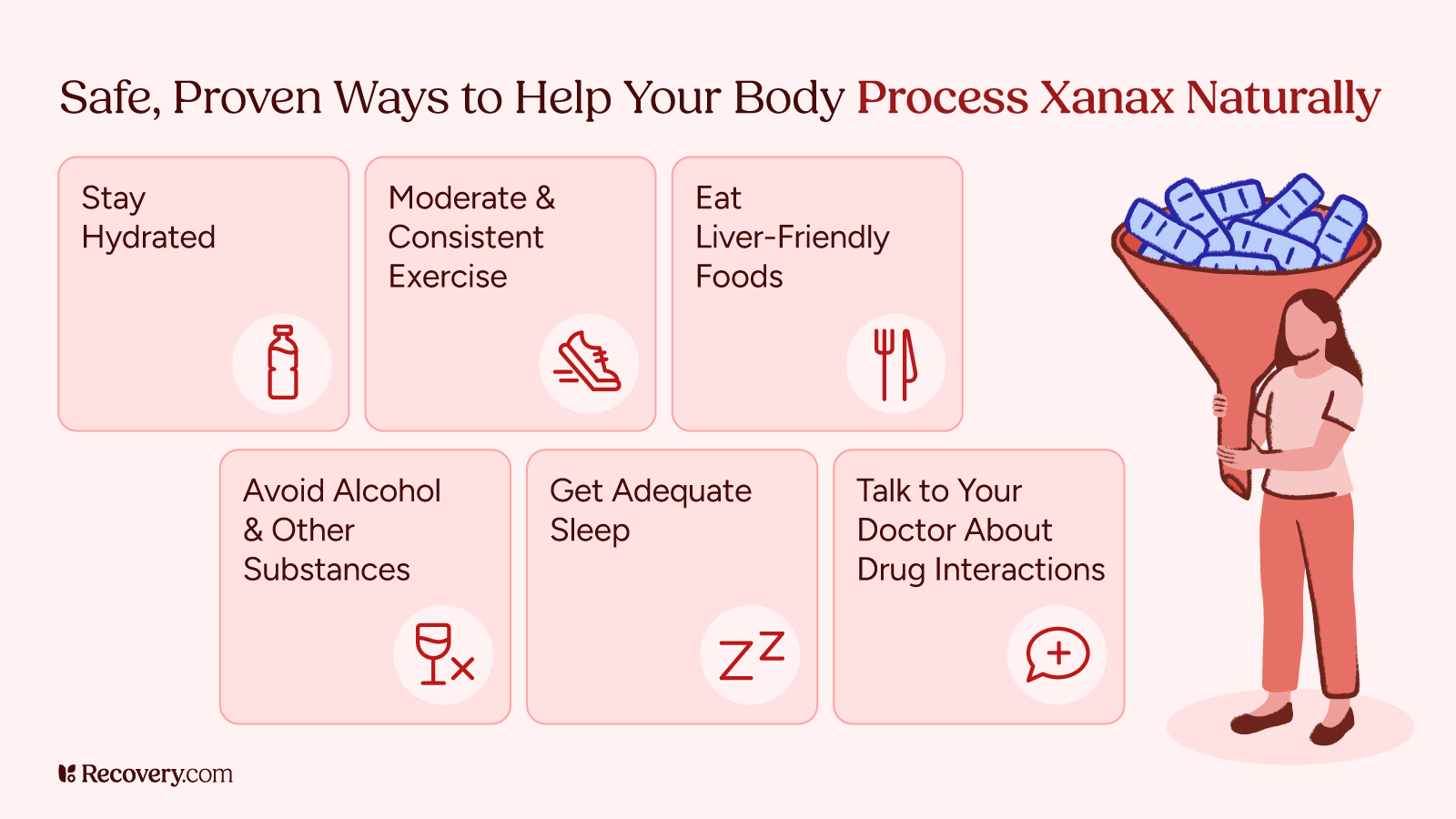
Safely Stopping Xanax Use
Never stop taking Xanax suddenly if you’ve been using it regularly. Abruptly stopping can trigger withdrawal symptoms that range from uncomfortable to dangerous, including intense cravings, rebound anxiety (which can be worse than your original anxiety), insomnia, irritability, muscle tension, and potentially seizures.16
Medical professionals recommend a gradual tapering schedule under supervision. Your prescribing doctor or a qualified treatment professional will create a personalized plan for your specific situation.
Always seek medical guidance for stopping Xanax—even if you’ve been taking it without a prescription or at higher doses than prescribed. Healthcare providers can safely manage your tapering process, adjust your plan if needed, and recommend treatments to ease your withdrawal symptoms.
Finding Support for Xanax Dependence
Knowing how long Xanax stays in your system is just one piece of a larger puzzle. If you’ve found yourself taking Xanax more frequently than prescribed, needing higher doses to get the same effect, or experiencing withdrawal symptoms when you try to stop, these may be signs of physical dependence.
Xanax dependence is a medical condition that requires proper detox and addiction treatment—not willpower alone.17 The good news is that effective, compassionate treatment options exist. With the right support, people can and do recover from benzodiazepine dependence every day.
Treatment for Xanax addiction typically involves a medically supervised tapering process combined with therapy to address any underlying anxiety or mental health concerns. This comprehensive approach helps not just with safely stopping Xanax, but also developing healthy coping strategies to avoid becoming addicted in the future.
If Xanax abuse has become a problem for you or someone you care about, effective treatment is available. Recovery.com can connect you with specialized centers experienced in benzodiazepine dependence treatment. Take the first step toward recovery by exploring treatment programs that match your specific needs and speaking with an admissions specialist today.
FAQs
-
1. Drug Enforcement Administration. (2020). Drug fact sheet: Benzodiazepines. U.S. Department of Justice. https://www.dea.gov/sites/default/files/2020-06/Benzodiazepenes-2020_1.pdf
-
2. Griffin CE 3rd, Kaye AM, Bueno FR, Kaye AD. Benzodiazepine pharmacology and central nervous system-mediated effects. Ochsner J. 2013 Summer;13(2):214-23. PMID: 23789008; PMCID: PMC3684331.
-
3. George TT, Tripp J. Alprazolam. [Updated 2023 Apr 24]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538165/
-
4. George TT, Tripp J. Alprazolam. [Updated 2023 Apr 24]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538165/
-
5. Qriouet Z, Qmichou Z, Bouchoutrouch N, Mahi H, Cherrah Y, Sefrioui H. Analytical Methods Used for the Detection and Quantification of Benzodiazepines. J Anal Methods Chem. 2019 Sep 5;2019:2035492. doi: 10.1155/2019/2035492. PMID: 31583157; PMCID: PMC6748181.
-
6. Qriouet Z, Qmichou Z, Bouchoutrouch N, Mahi H, Cherrah Y, Sefrioui H. Analytical Methods Used for the Detection and Quantification of Benzodiazepines. J Anal Methods Chem. 2019 Sep 5;2019:2035492. doi: 10.1155/2019/2035492. PMID: 31583157; PMCID: PMC6748181.
-
7. Nordal K, Øiestad EL, Enger A, Christophersen AS, Vindenes V. Detection Times of Diazepam, Clonazepam, and Alprazolam in Oral Fluid Collected From Patients Admitted to Detoxification, After High and Repeated Drug Intake. Ther Drug Monit. 2015 Aug;37(4):451-60. doi: 10.1097/FTD.0000000000000174. PMID: 25549207.
-
8. Concheiro, Marta*; Villain, Marion†; Bouchet, Stéphane‡; Ludes, Bertrand‡; López-Rivadulla, Manuel*; Kintz, Pascal‡. Windows of Detection of Tetrazepam in Urine, Oral Fluid, Beard, and Hair, With a Special Focus on Drug-Facilitated Crimes. Therapeutic Drug Monitoring 27(5):p 565-570, October 2005. | DOI: 10.1097/01.ftd.0000164610.14808.45
-
9. Qriouet Z, Qmichou Z, Bouchoutrouch N, Mahi H, Cherrah Y, Sefrioui H. Analytical Methods Used for the Detection and Quantification of Benzodiazepines. J Anal Methods Chem. 2019 Sep 5;2019:2035492. doi: 10.1155/2019/2035492. PMID: 31583157; PMCID: PMC6748181.
-
10. Ariella, R. (2021, May 4). Benzodiazepines and older adults: The impact of different metabolism. Benzodiazepine Information Coalition. https://www.benzoinfo.com/benzodiazepine-older-adults-impact/#differentmetabolism
-
11. Kraus, J. W., et al. “Effects of Aging and Liver Disease on Disposition of Lorazepam.” Clinical Pharmacology & Therapeutics, vol. 24, no. 4, Oct. 1978, pp. 411–19. DOI.org (Crossref), https://doi.org/10.1002/cpt1978244411.
-
12. Qriouet Z, Qmichou Z, Bouchoutrouch N, Mahi H, Cherrah Y, Sefrioui H. Analytical Methods Used for the Detection and Quantification of Benzodiazepines. J Anal Methods Chem. 2019 Sep 5;2019:2035492. doi: 10.1155/2019/2035492. PMID: 31583157; PMCID: PMC6748181.
-
13. Casati, Andrea, and Marta Putzu. “Anesthesia in the Obese Patient: Pharmacokinetic Considerations.” Journal of Clinical Anesthesia, vol. 17, no. 2, Mar. 2005, pp. 134–45. ScienceDirect, https://doi.org/10.1016/j.jclinane.2004.01.009.
-
14. George TT, Tripp J. Alprazolam. [Updated 2023 Apr 24]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538165/
-
15. Sustained-Release, Extended-Release, and Other Time-Release Formulations in Neuropsychiatry.” Psychiatrist.Com, https://www.psychiatrist.com/jcp/sustained-release-extended-release-release-formulations/
-
16. Pétursson H. The benzodiazepine withdrawal syndrome. Addiction. 1994 Nov;89(11):1455-9. doi: 10.1111/j.1360-0443.1994.tb03743.x. PMID: 7841856.
-
17. Dickinson B, Rush PA, Radcliffe AB. Alprazolam use and dependence. A retrospective analysis of 30 cases of withdrawal. West J Med. 1990 May;152(5):604-8. PMID: 2349800; PMCID: PMC1002418.
Our Promise
How Is Recovery.com Different?
We believe everyone deserves access to accurate, unbiased information about mental health and recovery. That’s why we have a comprehensive set of treatment providers and don't charge for inclusion. Any center that meets our criteria can list for free. We do not and have never accepted fees for referring someone to a particular center. Providers who advertise with us must be verified by our Research Team and we clearly mark their status as advertisers.
Our goal is to help you choose the best path for your recovery. That begins with information you can trust.