Do I Have Body Dysmorphia? 13 Signs You Shouldn’t Ignore



Dr. Jack Bartel (he/him) is a licensed clinical psychologist and LGBTQ+ health educator and consultant. He received his doctorate of clinical psychology from Florida Tech and completed his predoctoral internship at Jackson Memorial Hospital in Miami and his postdoctoral residency at the Orlando VA.

Dr. Mala, is the Chief Clinical Officer at Recovery.com, where she develops impartial and informative resources for people seeking addiction and mental health treatment.




Dr. Jack Bartel (he/him) is a licensed clinical psychologist and LGBTQ+ health educator and consultant. He received his doctorate of clinical psychology from Florida Tech and completed his predoctoral internship at Jackson Memorial Hospital in Miami and his postdoctoral residency at the Orlando VA.

Dr. Mala, is the Chief Clinical Officer at Recovery.com, where she develops impartial and informative resources for people seeking addiction and mental health treatment.
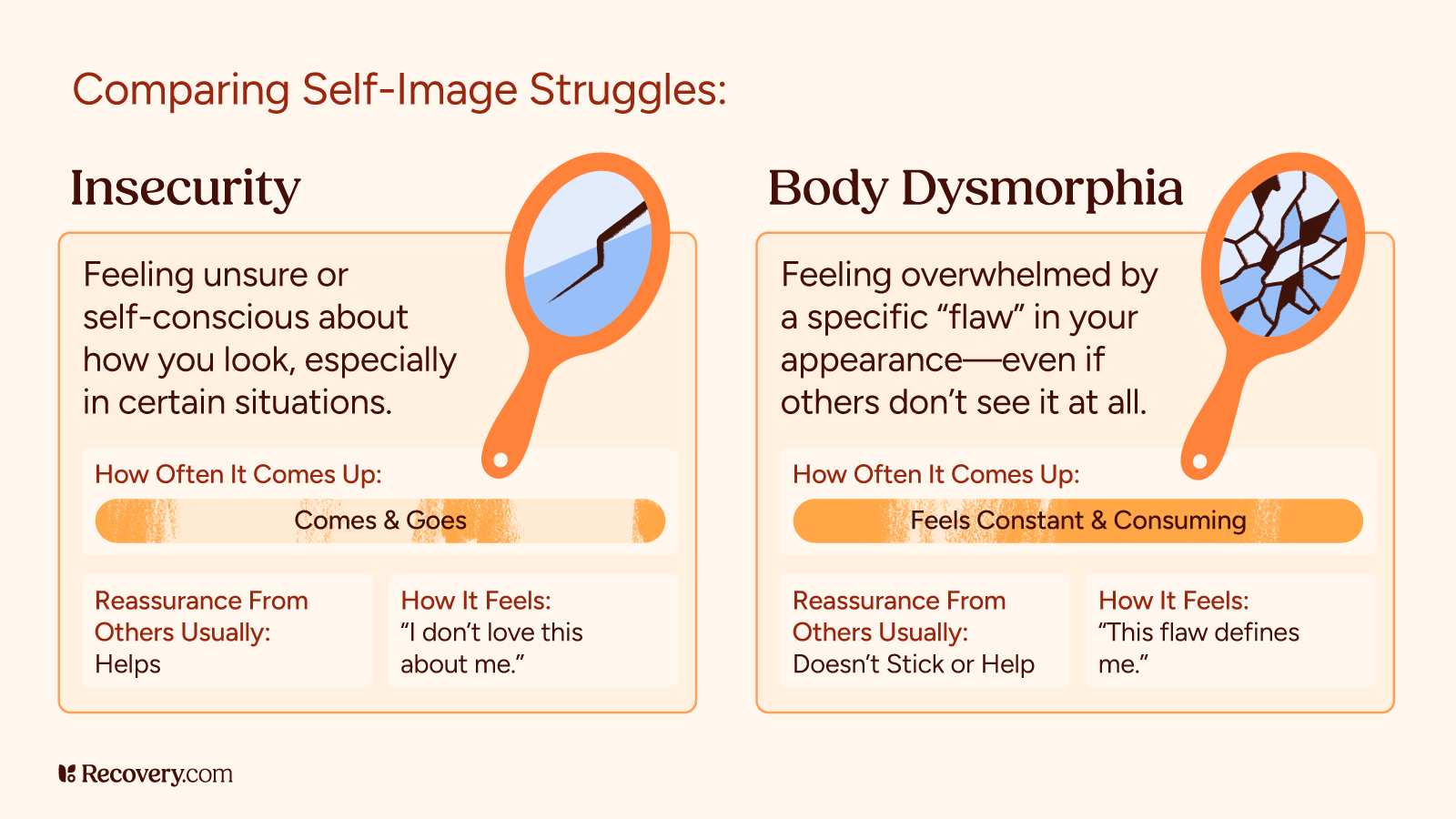
It’s normal to have days when we feel uncomfortable in our own skin. But for some, those feelings go far beyond everyday insecurity. If you find yourself obsessing over perceived flaws in your appearance—flaws that others may not even notice—you might be wondering if it’s something more serious.
Body dysmorphic disorder (BDD) is a mental health condition that affects the way people see and think about their bodies, often causing them significant distress and interfering with their daily life. In this article, we’ll explore what body dysmorphia really is, how to recognize the signs, and when it’s time to seek support.
What Is Body Dysmorphia?
Body dysmorphic disorder (BDD) is a mental health condition “where a person experiences a preoccupation with a perceived defect or flaw in one’s physical appearance when, in fact, they appear normal.”1
People with BDD tend to fixate on specific body parts or features, most commonly the skin, nose, hair, or body shape. This obsessive focus often leads to repeated behaviors such as mirror checking, grooming, or comparing themselves to others in an attempt to “fix” or hide the flaw. It can also cause the person a lot of stress.
What sets BDD apart from general body dissatisfaction is the intensity and persistence of these thoughts. The distress caused by the perceived imperfection can interfere with your daily life, relationships, and emotional well-being.
BDD isn’t just about wanting to look better or not being happy with a part of your body. It’s about feeling unable to stop thinking about the flaw, no matter how many times others reassure you or how much effort you put into changing it.
Signs and Symptoms of BDD
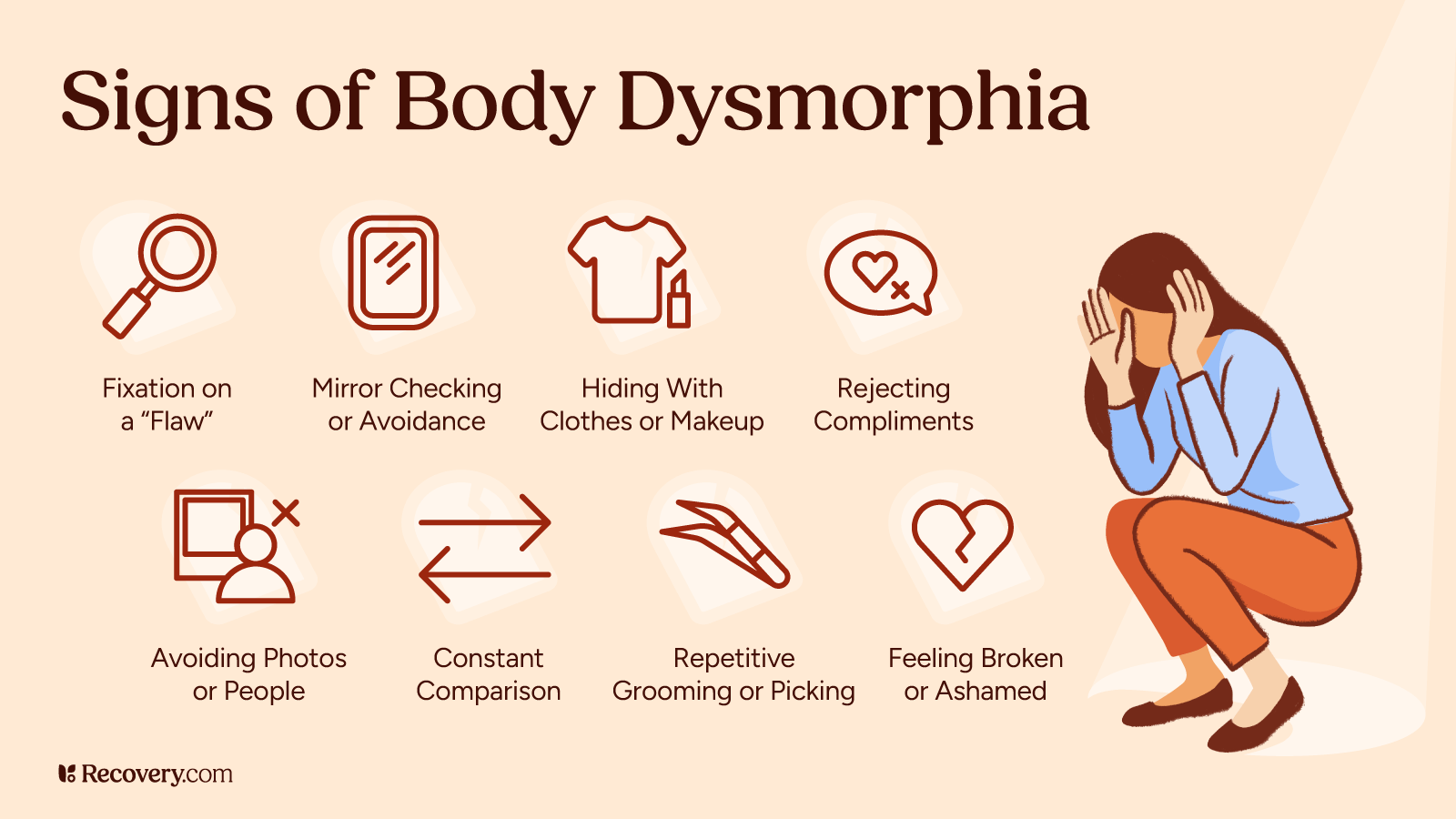
Many people struggle for years before realizing their intense appearance concerns have a name—recognizing these signs of BDD can be validating and the first step toward getting help:2
1. Excessive Worry About a Specific Part of the Body
People with BDD experience intense, uncontrollable worry about a particular body part. They feel unable to calm or manage these concerns, no matter how hard they try.
2. Hiding or Concealing Perceived Flaws
People with BDD go to great lengths to conceal the area they’re focused on. They use hats, scarves, makeup, strategic clothing, or certain hairstyles to mask or distract from the perceived imperfection.
3. Dismissing Compliments or Reassurances
It feels impossible to believe when loved ones say you look fine or beautiful. People with BDD often dismiss positive feedback, convinced that others are just being kind or dishonest.
4. Avoiding Social Situations
Intense self-consciousness or shame leads to skipping school, work, dates, or social events. The fear of being seen or judged becomes overwhelming and interferes with normal activities.
5. Feeling Distress Over Photos
Many people with BDD feel extreme anxiety or panic at the thought of having their picture taken. They fear that images will highlight or expose their perceived flaw to others.
6. Engaging in Repetitive Appearance-Related Behaviors
These behaviors include frequently checking mirrors or avoiding them entirely, skin picking, excessive grooming, or constantly trying to “fix” the perceived flaw. People may spend hours using makeup, adjusting clothing, or even seeking cosmetic procedures.
7. Seeking Constant Reassurance
People with BDD repeatedly ask friends, family, or even strangers for validation about their appearance. They hope to feel better, though any relief is typically short-lived and the need for reassurance returns quickly.
8. Constantly Comparing Yourself to Others
People with BDD obsessively compare their appearance to others on social media or in real life. These comparisons often leave them feeling inferior or deeply flawed, reinforcing their negative self-perception.
9. Feeling Defined by the Perceived Flaw
It’s common for someone with BDD to believe that their “flaw” makes them unlovable, broken, or even repulsive. This belief persists despite reassurances from others who don’t see the same imperfection.
10. Overexercising or Overtraining
Some people have muscle dysmorphia, which involves a preoccupation with the idea that their body build is too small or insufficiently muscular.3 This may lead to excessive exercise, steroid use, or unhealthy supplement usage in an attempt to control their body’s appearance.
11. Seeking Multiple Healthcare Providers
People with BDD visit numerous dermatologists, cosmetic surgeons, or other specialists in search of a “fix” for their perceived flaw. They continue this search even after being told repeatedly that nothing is wrong.
12. Undergoing Unnecessary Cosmetic Procedures
Some people pursue plastic surgery or aesthetic treatments that aren’t medically needed. These procedures rarely provide lasting relief and may worsen distress when the results don’t “solve” the internal struggle, often causing the obsession to shift to different body parts.
13. Having Thoughts of Self-Harm or Suicide
In severe cases, the emotional pain becomes overwhelming and leads to feelings of hopelessness and worthlessness. Some people may experience thoughts of self-harm or suicide as a way to escape the distress caused by their body image concerns.
Thoughts of suicide and self-harm are serious warning signs that should never be ignored. If you or someone you know is experiencing these thoughts, seek immediate help by calling the 988 Suicide & Crisis Lifeline (call or text 988) or contact your local emergency services. Remember that these feelings are symptoms of the disorder, not a reflection of reality, and professional help can provide relief.
Could I Have Body Dysmorphia? A Quick Self-Reflection Quiz
This brief quiz is based on common diagnostic criteria and clinical observations from the DSM-5-TR used to identify body dysmorphic disorder (BDD).4 It’s not a diagnostic tool, but it can help you reflect on whether your body image concerns may warrant further support from a mental health professional.
Instructions
For each statement, answer Yes or No.
- Do you often worry about a specific part of your appearance that others say looks fine or don’t seem to notice?
- Do you frequently check mirrors, photos, or reflective surfaces to look at this area of concern?
- Do you avoid social situations, photos, or video calls because of how you feel about your appearance?
- Do you spend more than an hour a day thinking about your appearance or trying to “fix” your flaw?
- Have you tried to hide or cover up this part of your body with makeup, clothing, or accessories?
- Do you seek frequent reassurance from others about how you look, but rarely feel reassured?
- Have you seen multiple doctors, dermatologists, or plastic surgeons about this concern?
- Have you ever felt hopeless, depressed, or had thoughts of self-harm related to your appearance?
Scoring
- 0–2 “yes” answers: You may have occasional appearance concerns, which are common.
- 3–5 “yes” answers: Your concerns might be affecting your quality of life. It may be helpful to talk to a therapist.
- 6+ “yes” answers: You may be experiencing signs consistent with body dysmorphic disorder. Consider seeking professional support.
Note: This quiz is inspired by theBody Dysmorphic Disorder Questionnaire (BDDQ) and clinical criteria in the DSM-5. It is for educational use only and is not a substitute for a professional diagnosis.
What Causes Body Dysmorphic Disorder?
The exact cause of body dysmorphic disorder (BDD) is not fully understood, but several risk factors are believed to contribute:5
- Genetics: A family history of BDD, obsessive-compulsive disorder (OCD), or other mental health conditions may increase the risk.
- Brain chemistry: Imbalances in serotonin, a neurotransmitter that affects mood and anxiety, may play a role.
- Trauma or bullying: Negative experiences, such as childhood trauma or being bullied for appearance, can increase the likelihood of developing BDD.
- Cultural factors: Societal pressures and unrealistic beauty standards in media can exacerbate body image concerns and may contribute to the development of BDD.
When Should You Seek Help?
If you’re experiencing any of the signs or symptoms of body dysmorphic disorder (BDD), it’s important to know that you don’t have to manage it alone. While everyone has moments of insecurity or self-doubt, BDD can be overwhelming and may require professional support to manage.
Here are some signs that it’s time to seek help:
The Distress Affects Your Daily Life
If your preoccupation with your appearance is interfering with your ability to work, study, maintain relationships, or enjoy social activities, it’s a clear indication that your body image concerns may be more than just a passing insecurity.
Repetitive Behaviors Are Difficult to Control
If you find yourself unable to stop behaviors like mirror checking, skin picking, or seeking constant reassurance, and these actions are consuming a significant amount of time each day, it might be time to reach out for help.
Seeking Medical or Cosmetic Treatments Does Not Bring Relief
If you’ve tried multiple cosmetic procedures, seen various healthcare providers, or spent significant time and money trying to “fix” a perceived flaw, but continue to feel unsatisfied or worse, this is a signal that the issue is rooted in a deeper psychological concern, not a physical flaw.
Reassurance From Others Doesn’t Ease Your Anxiety
If loved ones consistently reassure you that you look fine or that your concerns are unfounded, but you continue to feel distressed, it may indicate the need for professional intervention. BDD is not about vanity—it’s a mental health issue that requires treatment.
Self-Harm or Suicidal Thoughts Arise
If you experience thoughts of self-harm or suicide due to your appearance or body image distress, it is critical to seek immediate support. These thoughts are a sign of the severe emotional toll BDD can have and should be addressed by a mental health professional right away.
How Is BDD Treated?
Seeking help is a positive step toward healing. Body dysmorphic disorder (BDD) can be a challenging condition to manage on your own, but effective treatment options are available.6 The goal of treatment is to help people recognize and address the distorted thoughts and behaviors that fuel their distress, allowing them to improve their quality of life.
Common treatment approaches for BDD include:
Cognitive Behavioral Therapy (CBT)
Cognitive behavioral therapy helps people challenge distorted thoughts and behaviors related to their body image concerns. This evidence-based approach teaches patients to recognize and change negative thought patterns that fuel their distress.
Medication
Medication can be a helpful part of treatment, particularly when someone also has symptoms of related disorders like anxiety, depression, or obsessive-compulsive disorder (OCD), which often co-occur with BDD. Psychiatrists also commonly prescribe a class of antidepressants called selective serotonin reuptake inhibitors (SSRIs) to help manage these symptoms. While medication can provide relief from the emotional distress and obsessive behaviors associated with BDD, it’s usually most effective when combined with psychotherapy.
Support Groups
Participating in support groups can be beneficial for people struggling with BDD. Being able to share experiences with others who understand the challenges of living with BDD provides emotional support and a sense of community. These groups offer a safe space to discuss body image struggles and help people feel less isolated in their journey toward recovery.
Family Therapy & Education
BDD can significantly impact your relationships, making it incredibly helpful to involve family members in the treatment process. Family therapy helps your loved ones understand the condition and learn how to provide positive, supportive responses. Educating family members about the nature of BDD reduces misunderstandings and helps them better support your recovery journey.
Lifestyle Changes
Exercise, mindfulness, and relaxation techniques can help manage the anxiety and stress that often accompany BDD. Regular physical activity improves mood, boosts self-esteem, and reduces compulsive behaviors. Mindfulness practices such as meditation or deep breathing exercises help individuals manage intrusive thoughts and stay grounded in the present moment, rather than becoming fixated on appearance-related concerns.
Discover a Path to Healing
From intensive individual therapy programs to 24/7 structured support, the right solution is out there. Explore options for wellness-focused mental health treatment, trauma treatment centers, and more to find a safe space to heal. Find a mental health facility today and begin your journey toward stability and peace.
FAQs
-
Nicewicz HR, Torrico TJ, Boutrouille JF. (2024, January 20). Body Dysmorphic Disorder. https://www.ncbi.nlm.nih.gov/books/NBK555901/
-
Singh AR, Veale D. (2019, January). Understanding and treating body dysmorphic disorder. https://pubmed.ncbi.nlm.nih.gov/30745686/
-
Pope, Harrison G., et al. (1997, November). “Muscle Dysmorphia: An Underrecognized Form of Body Dysmorphic Disorder. https://doi.org/10.1016/S0033-3182(97)71400-2.
-
Substance Abuse and Mental Health Services Administration. (2016, June). DSM-5 Changes: Implications for Child Serious Emotional Disturbance. https://www.ncbi.nlm.nih.gov/books/NBK519712/table/ch3.t19/
-
Feusner JD, Neziroglu F, Wilhelm S, Mancusi L, Bohon C. (2010, July 1). What Causes BDD: Research Findings and a Proposed Model. https://pmc.ncbi.nlm.nih.gov/articles/PMC3859614/
-
Phillips, Katharine A. (2005). The Broken Mirror: Understanding and Treating Body Dysmorphic Disorder. https://psycnet.apa.org/record/2005-07388-000
Our Promise
How Is Recovery.com Different?
We believe everyone deserves access to accurate, unbiased information about mental health and recovery. That’s why we have a comprehensive set of treatment providers and don't charge for inclusion. Any center that meets our criteria can list for free. We do not and have never accepted fees for referring someone to a particular center. Providers who advertise with us must be verified by our Research Team and we clearly mark their status as advertisers.
Our goal is to help you choose the best path for your recovery. That begins with information you can trust.