Complex PTSD: How I’m Recovering My Ability to Self-Regulate



Located in Portland, OR, Olivia Pennelle (Liv) is an experienced writer, journalist, and coach. She is the founder of the popular site Liv’s Recovery Kitchen, a site dedicated to helping people flourish in their recovery.




Located in Portland, OR, Olivia Pennelle (Liv) is an experienced writer, journalist, and coach. She is the founder of the popular site Liv’s Recovery Kitchen, a site dedicated to helping people flourish in their recovery.
I’ve spent a lifetime being told that I’m hyper-sensitive, that I overreact to situations, that I’m difficult to manage, or that I want to be on my own too much.
Unbeknown to me, I have been suffering with a debilitating condition that stretches back to childhood. Had I not undertaken the overwhelmingly stressful move to America, I may have remained unconscious to symptoms that have run havoc throughout my life, my body, my relationships, and my ability to relate to the world.
At six years sober, I was diagnosed with Complex PTSD.
What is Complex PTSD?
Most traumatic events are on-off or time-limited, such as a car accident, rape, or natural disasters.
According to The National Center for PTSD, people with Complex PTSD experience chronic trauma that continues or repeats for months or years at a time. The types of trauma that are associated with Complex PTSD include long-term domestic abuse, long-term child physical and sexual abuse, prostitution brothels, prisoner of war camps, and concentration camps.
Even though 92 percent of those with Complex PTSD meet the diagnostic criteria for PTSD, they do exhibit additional symptoms which affect their self-concept and how they deal with stressful events.
Classic symptoms of those with the disorder include difficulties with emotional regulation, consciousness, self-perception, distorted perceptions of the perpetrator, relations with others, and a sense of meaning in life.
Discovering Complex PTSD in My Life
For as long as I can remember, I’ve exhibited certain behaviors that I just thought were quirks of my personality – or my being “overly sensitive.” I now see that not only was I suffering with repeated traumas, I was also displaying symptoms of this disorder.
My traumas began in childhood and I suffered with repeated traumatic events throughout my adult life…until I found recovery. My ability to adapt to stressful situations is perhaps the most compromised of all my symptoms. What stands out most are these characteristics:
- I jumped every time I heard a loud noise.
- I’ve always had to leave noisy rooms.
- I’ve never felt safe my entire life.
- I’ve always felt trapped – in my body, and in situations with others.
- I’ve always slept on the side of the bed closest to the door.
- Raised voices brought about a sense of panic, not knowing whether to run or freeze.
- I have no recollection of my childhood before the age of five or six years old.
- I have a long history of self-destructive behaviors, using drugs, alcohol, food, and even sex to take the edge off my reality.
- I always picked relationships with emotionally unavailable people who would treat me badly – blaming myself for the inevitable outcome.
- Most family members brought on symptoms of acute anxiety, increased my desire to use substances, and drained me of energy.
- I have felt numb to my body for most of my life.
The Lingering Desire to Numb
In his book The Body Keeps the Score, renowned trauma specialist Bessel A. van der Kolk, says:
“Traumatized people chronically feel unsafe inside their bodies: The past is alive in the form of gnawing interior discomfort. Their bodies are constantly bombarded by visceral warning signs, and, in an attempt to control these processes, they often become expert at ignoring their gut feelings and in numbing awareness of what is played out inside. They learn to hide from their selves.”
Even though I found recovery, the desire to numb or disassociate, has never really gone away because I was faced with an un-anaesthetized and very uncomfortable reality. It was like the lights were turned on and the noise turned up. All of these symptoms remained throughout my recovery. They have lessened considerably, given my dedication to self-care, but they were still present. I’ve continued to use food, TV, and relationships to avoid my reality in varying degrees. And I’ve still had a visceral reaction to stressful events, often feeling completely agitated in my body and overwhelmed with emotion.
Moving to America caused such a stress reaction in my body that, after the adrenaline that kept me going finally wore off, I returned to my body’s pre-recovery state and began to physically shut down. My body and mind were exhausted. Last year, I spent most days relying on coffee and carbohydrates to try and get through the day. I suffered with recurrent depression, constant headaches, and had pain throughout my body.
My doctor just kept prescribing different anti-depressant medication, told me I was stressed and run down, and told me to exercise and lose weight. I already excessively exercised, only to get temporary relief followed by even more exhaustion.
Whatever I was doing wasn’t working.
Recovering From PTSD
Thoroughly fed up with my chronic fatigue, and with a distinct feeling the answer was much deeper, I visited a naturopathic doctor in January. That decision changed my life. Through her intervention, diagnostic testing, and treatment, we realized that I was in acute adrenal fatigue and my body was completely dysregulated. I was unable to effectively process stress, I had markers of an autoimmune condition, and I had inflammation throughout my body.
The only answer was to stop, process, and learn how to better regulate. I started on an adrenal recovery protocol, including steroids, and began taking restorative activities seriously. With much research into the correlation between adrenal fatigue and addiction, I realized the need to work with a therapist. We uncovered a vast history of repeated trauma, emotional repression, and we began working within a complex PTSD framework for trauma healing.
The Results
The past six months of therapy has achieved more than my six years in recovery! I finally feel like I know who I am, why I act the way that I do, and that there is more to recovery than I had experienced. I have started to thrive in ways I never realized were possible. It hasn’t been easy, though. It has required twice-weekly therapy, regular visits to my doctor, extensive reading, soul-searching, and lots and lots of healing, sobbing tears.
Dr. Judith Herman of Harvard University says that recovery from Complex PTSD requires restoration of control and power for the traumatized person. She contends that survivors can become empowered by healing relationships which create safety, allow for remembrance and mourning, and promote reconnection with everyday life.
Much of my work has involved empowering myself and gaining agency: learning about female architypes, reconnecting to the feminine and nature, drawing on sources of energy, learning about the psyche and splits within it, and digging into my core strengths and capacity to regulate. I’ve also spent a long time looking at which relationships drain my energy and disempower me, and those that harm me. I have also worked hard to enforce stronger boundaries – putting myself, my healing, and my well-being before the needs of anyone else.
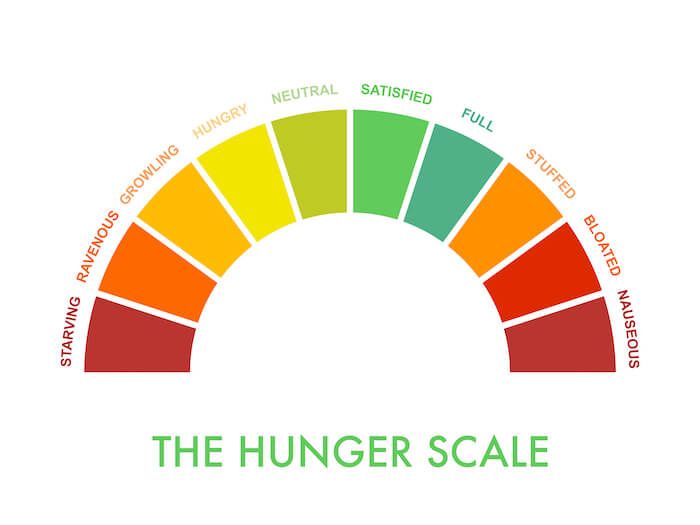
That doesn’t mean I’m healed. There are still months – if not years – of work to do. Trauma therapy takes a long time. It is painstaking work. And there are times that I suffer with complete dysregulation in my body when I am triggered. In fact, I was triggered just a few weeks ago and it felt so completely overwhelming that it affected my ability to work, sleep, relax, eat, and my body felt like it was re-experiencing trauma. During these times, I have to remind myself that I have the tools to quickly regulate my nervous system and emotions and express the stress hormones out of my body.
These are my go-to tools:
- Strenuous exercise
- Cycling to the top of a nearby mountain to be in the trees
- Meditation for relaxation and Metta practice
- Meditation community
- Qigong
- Acupuncture
- Therapy
- Yin and restorative yoga
- Naturopathic stress supplements
- Calming music
- Turning off devices
- Aromatherapy
- Sleep
- Nurturing food
- Little or no caffeine
Triggering events like the one I recently experienced remind me that, much like addiction recovery, the process isn’t linear. We often have set backs and we also have huge leaps of growth. I know there is much work left to do – and I wonder if we ever stop uncovering these pains – but at the same time, I have never felt freer, more alive, more connected to my body.
I’m excited to see what lies ahead. As devastating and dysregulating as trauma can be, I wouldn’t have recovered into the woman I am without it.
Our Promise
How Is Recovery.com Different?
We believe everyone deserves access to accurate, unbiased information about mental health and recovery. That’s why we have a comprehensive set of treatment providers and don't charge for inclusion. Any center that meets our criteria can list for free. We do not and have never accepted fees for referring someone to a particular center. Providers who advertise with us must be verified by our Research Team and we clearly mark their status as advertisers.
Our goal is to help you choose the best path for your recovery. That begins with information you can trust.