More About Rehabs Accepting Aetna
Aetna is one of the largest health insurance providers in the United States, and many drug and alcohol rehab centers accept Aetna insurance.(1)
With Aetna coverage, some or all of your addiction treatment costs could be covered, depending on your specific plan and policy.(2) However, it can be difficult to know which centers are the best fit for your needs and what services your insurance will support.
Does Aetna Cover Addiction and Mental Health Treatment?
Aetna may cover some degree of drug and alcohol rehab, though costs may vary.(3)
The Affordable Care Act (ACA) of 2010 expands your access to care for essential health benefits, including SUD and mental health services.(4) Under this law, marketplace health insurance companies must cover at least some of the costs for the medically necessary treatment of essential health benefits.(5)
That said, your level of coverage can vary depending on your specific policy.(5) Verifying your insurance before committing to treatment is essential. It can help you understand your benefits and the level of Aetna coverage for drug rehab you’ll receive.
Which Types of Addiction and Mental Health Treatment Does Aetna Cover?
Aetna covers addiction and mental health services in multiple treatment settings.(3)
Addiction and mental health treatment looks different for everyone.(6) Some may need more in-depth treatment approaches, while standard care might work for others.(6) That’s why several levels of care are available with individualized treatment plans to meet you where you are in recovery.
Here are some common types of addiction treatment a rehab that takes Aetna may offer:(6)
- Detox: Detox is often the first step in treatment for many before transitioning to another level of care. People attend detox to rid their bodies of substances under continuous medical supervision. Medical professionals may administer medications to ease cravings and the withdrawal process based on your situation.
- Inpatient/residential programs: These programs provide a safe, supportive living environment with 24/7 support during treatment. Addiction and mental health professionals use evidence-based therapeutic interventions, like cognitive behavioral therapy (CBT) and motivational interviewing (MI), to help you address the underlying causes of mental health conditions and gain coping skills.
- Outpatient programs: With outpatient care, you can live at home and attend treatment. Various levels of outpatient care are available, including partial hospitalization programs (PHPs), intensive outpatient programs (IOPs), and standard ones. Each differs in intensity and required attendance frequency but offers similar approaches to inpatient rehab.
- Aftercare: Mental health professionals agree that remaining in care after completing an initial program benefits long-term recovery. Some common types of addiction aftercare include ongoing therapy, sober living homes, and 12-Step programs.
Does Aetna Cover Co-Occurring Disorder Treatment?
Yes, Aetna may also cover co-occurring disorder treatment to some level.
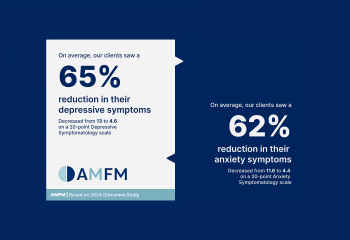
Many people with with mental health disorders, such as anxiety, depression, and post-traumatic stress disorder (PTSD), also struggle with a substance use disorder (SUD), or addiction.(7)
Mental health professionals recommend treating both conditions in tandem with an integrated approach to promote long-term recovery.(6)
Since mental health care is an essential health benefit under the ACA, you could receive partial or full coverage for co-occurring disorder treatment costs at a rehab that takes Aetna.
Aetna and Medically-Assisted Treatment
MAT is a form of rehab that combines medication with therapy to help those recovering from addiction. Aetna insurance covers many forms of MAT, including methadone and buprenorphine.
Do Treatment Centers Need to Be In-Network?
Aetna insurance plans may cover out-of-network rehab, but the specific coverage will depend on the individual's insurance plan and policy.
Some Aetna plans have out-of-network benefits that allow members to receive coverage for services from providers that are not in the plan's network.
However, this coverage is usually at a lower level than in-network coverage, and members may have to pay more out-of-pocket costs.
How to Use Aetna for Addiction and Mental Health Treatment
Using Aetna coverage for addiction treatment can be simple. It starts with verifying your insurance to understand which in-network providers are available.(3)
You can contact Aetna by phone or log into your patient portal on their website to learn more about your benefits.(3)
When you call Aetna’s toll-free number on your member ID card, they connect you with an Aetna Care Advocate.(3) Your advocate can help you determine your recovery goals and offer guidance on finding appropriate care.(3) They’re there every step of the way to ensure you find a facility that works for your situation.(3)
Sources:
- Aetna. (n.d.). Your mental health & well-being.
- Aetna. (n.d.). ACA health insurance plan coverage.
- Aetna. (n.d.). If you’re struggling with drugs or alcohol, Aetna can help.
- HealthCare.gov. (n.d.). Affordable Care Act (ACA).
- HealthCare.gov. (n.d.).Essential health benefits.
- National Institute on Drug Abuse. (2018). Principles of drug addiction treatment: A research-based guide (third edition).
- National Alliance on Mental Illness. (n.d.). Substance use disorders.